Is insulin resistance common after pregnancy?
Unfortunately, yes. Research shows that becoming insulin resistant is not just a pregnancy-related condition—it often continues into the postpartum period, especially in women who had gestational diabetes (GDM). But here’s what most postpartum women aren’t told: ongoing insulin resistance after birth can silently sabotage your energy, weight, mood, and even milk supply (Source).
Insulin resistance postpartum can be influenced by various factors beyond gestational diabetes. Hormonal fluctuations after delivery, including changes in estrogen, progesterone, and cortisol levels, can impact how your body responds to insulin. Additionally, the stress of caring for a newborn, disrupted sleep patterns, and changes in physical activity levels can all contribute to maintaining or worsening insulin resistance during this period.
Moreover, insulin resistance postpartum is not only a concern for women with previous GDM; even those without a history of gestational diabetes may experience impaired insulin sensitivity due to genetic predispositions or lifestyle factors. It is important to recognize that insulin resistance can persist silently without obvious symptoms, making regular monitoring and early intervention crucial for long-term health.
Addressing insulin resistance postpartum involves a multifaceted approach, including adopting a balanced diet rich in whole foods, engaging in regular physical activity tailored to postpartum recovery, managing stress effectively, and ensuring adequate sleep. These strategies can help improve insulin sensitivity, support weight management, and enhance overall well-being during the postpartum period.
Understanding Insulin Resistance Postpartum
Insulin resistance occurs when your cells stop responding properly to insulin—the hormone responsible for regulating blood sugar. Your body compensates by producing more insulin, but over time, this leads to hormonal imbalance, inflammation, and exhaustion. The pancreas increases insulin production to try to maintain normal blood glucose, but sometimes it cannot produce enough insulin, resulting in high blood sugar.
In pregnancy, insulin resistance naturally increases. For some women, especially those with GDM, this resistance doesn’t resolve postpartum. Women with certain genetic backgrounds—several genes have been linked to insulin resistance—may be at higher risk for developing insulin resistance after pregnancy. One study found that over 50% of women who had gestational diabetes developed abnormal glucose metabolism within 5 years postpartum—with insulin resistance as a key driver (Source).
Introduction to Insulin Resistance
Insulin resistance is a condition where your body’s cells—especially muscle and fat cells—don’t respond as well as they should to insulin, the hormone that helps move glucose from your blood into your cells for energy. When this happens, your pancreas makes more insulin to try to keep your blood sugar in a healthy range. Over time, this can lead to higher insulin levels and eventually, higher blood glucose levels.
You don’t have to have diabetes to be affected by insulin resistance. In fact, many people experience impaired insulin sensitivity without realizing it, especially after major life events like pregnancy. Insulin resistance can impact your energy, mood, weight, and even your risk for chronic illness. Understanding how your body responds to insulin is the first step toward making food choices and lifestyle changes that support your health—now and in the future.
The Importance of Insulin Sensitivity
Insulin sensitivity is the opposite of insulin resistance—it means your cells respond well to insulin, allowing your body to absorb blood glucose efficiently and keep your blood sugar levels steady. When your insulin sensitivity is high, your pancreas doesn’t have to work overtime to release insulin, and your body can use carbohydrates from food for energy without causing a spike in blood glucose.
Why does this matter? Good insulin sensitivity supports a steadier rise and fall in blood sugar after eating, which helps you feel more energized, focused, and emotionally balanced. It also reduces your risk of developing high blood pressure, heart disease, and type 2 diabetes down the road. By supporting your insulin sensitivity with a healthy diet, regular physical activity, and stress management, you’re investing in your long-term well-being.
Symptoms of Insulin Resistance Postpartum
Wondering if your postpartum symptoms could be linked to insulin resistance? Common signs include:
- Fatigue that doesn’t improve with rest
- Cravings for sugar or carbs
- Brain fog or trouble focusing
- Weight retention (especially around the belly)
- Mood swings or anxiety
- Skin tags or dark patches of skin
- Low milk supply
- Difficulty losing weight despite “doing everything right”
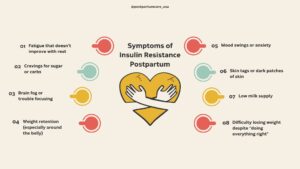
Not everyone who experiences these symptoms will have insulin resistance or develop diabetes, but these signs—especially when combined with high blood sugar—warrant further investigation.
If you’re nodding along, it’s not in your head. It’s hormonal.
Can Insulin Resistance Affect Milk Supply?
Yes—insulin plays a role in lactation. Emerging research suggests a link between insulin resistance and low milk supply, especially in women with PCOS or postpartum hormone imbalances. If you’re struggling to produce milk despite pumping, latching, and lactation support, insulin resistance may be an overlooked root cause.
Insulin is not only crucial for regulating blood sugar but also influences the function of mammary glands. Proper insulin sensitivity helps support the hormonal environment necessary for milk production. When cells become insulin resistant, the signaling pathways that promote lactation can be disrupted, potentially leading to reduced milk synthesis and secretion.
Furthermore, insulin resistance can affect other hormones involved in lactation, such as prolactin and oxytocin, which are essential for milk production and ejection. Imbalances in these hormones, combined with insulin resistance, may contribute to difficulties in establishing or maintaining an adequate milk supply.
Women with conditions like polycystic ovary syndrome (PCOS), which is often associated with insulin resistance, may be particularly vulnerable to lactation challenges. Additionally, postpartum hormonal fluctuations can exacerbate insulin resistance, further impacting milk supply.
Addressing insulin resistance through dietary changes, physical activity, and medical support when necessary may improve insulin sensitivity and help restore healthy milk production. If you suspect insulin resistance is affecting your breastfeeding journey, discussing this with your healthcare provider or lactation consultant can lead to targeted interventions that support both your metabolic health and lactation success.
What Causes Insulin Resistance After Pregnancy?
Postpartum insulin resistance can be triggered by:
- History of gestational diabetes
- Hormonal shifts (especially cortisol and estrogen)
- Blood sugar instability
- Inflammation or poor gut health
- Sleep deprivation
- Highly processed, low-nutrient diets
- Chronic stress or nervous system dysregulation
Your body just went through one of the most demanding events of its life—birth. If it’s struggling to regulate blood sugar now, it’s not a failure. It’s a signal that your body needs support.
The Long-Term Risks of Untreated Insulin Resistance
If left unaddressed, postpartum insulin resistance can increase your risk of:
- Type 2 diabetes
- Cardiovascular disease
- Fatty liver disease
- Fertility issues
- Weight gain and metabolic syndrome
A 2020 study confirmed that insulin resistance doesn’t just “go away” for many women after pregnancy—especially those who had GDM. It often progresses over time and contributes to long-term metabolic disorders unless it’s addressed early.
Is Insulin Resistance Reversible After Pregnancy?
In most cases—yes. The key is identifying it early and addressing the root causes. At Postpartum Care USA, we start with personalized lab testing to assess insulin levels, blood sugar regulation, cortisol, thyroid function, and nutrient deficiencies. Then, we create a targeted care plan that includes:
A blood sugar-friendly diet for insulin resistance
- (Think: more whole foods, fiber, protein, healthy fats, and reducing processed options—not restriction or extremes)
Key supplements to support insulin sensitivity
- Including magnesium, inositol, berberine, and omega-3s (based on your labs)
Nervous system support
- Because stress and cortisol are major contributors to blood sugar issues
- Gentle movement and sleep strategies
- That work with your lifestyle as a new mom—not against it
In some cases, medication may be recommended to help manage insulin resistance if lifestyle changes are not enough.
Food for Insulin Resistance Recovery
You don’t need to eat perfectly to heal, but nourishing your body matters. Choosing complex carbohydrates and managing your carbohydrate intake can support insulin sensitivity and help prevent insulin resistance from progressing to type 2 diabetes. Including a variety of food groups—such as fruits, vegetables, whole grains, proteins, and healthy fats—can help maintain balanced blood sugar levels.
Consider adding the following foods to your diet to help improve insulin sensitivity and regulate blood sugar levels:
- Leafy greens (like spinach, kale, arugula)
- High-quality protein (chicken, eggs, grass-fed beef, lentils)
- Healthy fats (avocados, olive oil, chia seeds)
- Low-glycemic fruits (berries, apples, pears)
- Resistant starches (like cold potatoes, cooked oats, or quinoa)
Be mindful to limit added sugars and manage your sugar intake to prevent spikes in blood sugar.
This is about nourishment, not punishment.
Weight Loss and Insulin Resistance
If you’re struggling to lose weight postpartum, insulin resistance could be playing a role. When your body is insulin resistant, it tends to store more energy as fat—especially around the belly—even if you’re eating healthy foods and staying active. High insulin levels make it harder for your body to burn fat for fuel, which can stall weight loss and leave you feeling frustrated.
The good news? You can treat insulin resistance and support weight loss by focusing on a balanced diet rich in whole grains, lean poultry, non starchy vegetables, and healthy fats, while limiting processed foods, added sugar, and unhealthy fats like saturated fats. Gentle movement, like walking or yoga, can also help improve insulin sensitivity and support your body’s ability to use glucose for energy. Remember, losing weight with insulin resistance is possible—it just takes a different approach than traditional dieting.
Preventing Insulin Resistance
Preventing insulin resistance starts with small, sustainable changes to your daily routine. Prioritize eating foods that are minimally processed, like whole grains, fresh vegetables, lean proteins, and healthy fats. Try to limit highly processed foods, white bread, processed starches, canned fruits in syrup, and foods high in added sugar or unhealthy fats.
Physical activity is another powerful tool—regular movement helps your muscle cells absorb blood glucose more efficiently, reducing the demand on your pancreas to produce more insulin. Managing stress, getting enough sleep, and maintaining a healthy weight are also key factors in reducing insulin resistance and supporting normal blood glucose levels. By making these food choices and lifestyle changes, you can lower your risk of developing insulin resistance and protect your long-term health.
You Deserve Answers—Not More Dismissal
If you’ve ever been told “it’s just postpartum” or blamed for not bouncing back, we want you to know: you’re not broken, and you’re not lazy. Insulin resistance is real, and with the right care, it’s reversible.
Need help getting to the root of your postpartum symptoms?
Comment CARE on our latest Instagram post or book a call to learn how our expert team can support your healing with lab-based, personalized postpartum care.
Pin This for Later:



Postnatal Depletion
Meet the Team
Our Services
Supplements
A virtual healthcare clinic that helps postpartum mamas recover from postnatal depletion syndrome with a holistic approach.

Get in touch