Motherhood is often described as one of the most joyful seasons of life. But for many women, it can also be one of the most isolating and emotionally complex.
While it’s normal for new moms to experience mood changes, fatigue, and moments of overwhelm, some women experience darker thoughts that go far beyond the typical “baby blues.”
These may include intrusive thoughts of harm, feelings of hopelessness, or even suicidal thoughts as a new mom.
If you’ve experienced this, you are not a bad mom. You are experiencing symptoms of a mental illness brought on by hormone changes and your body’s recalibration to life with a baby. And it can be treated with the right support.
Does Postpartum Depression Include Suicidal Thoughts?
Yes — while not every woman with postpartum depression experiences suicidal ideation, research shows that suicide is one of the leading causes of maternal death in the first year after giving birth.
A 2022 review published in Current Psychiatry Reports (Chin et al.) found that suicide accounts for approximately 20% of postpartum deaths, making it one of the top contributors to maternal mortality. The researchers emphasize that this period — pregnancy through the first 12 months postpartum — is not a time of “protection” for mental health, as once believed. In fact, it’s often a time of heightened vulnerability due to hormonal shifts, chronic sleep deprivation, social isolation, and untreated mental health conditions.
Another population-based study from the MGH Center for Women’s Mental Health found that suicidal behavior most often occurs 9–12 months postpartum, long after most women have been “cleared” by their OB and are no longer routinely screened for mood disorders.
This gap in care means that many new mothers suffering from severe depression or suicidal ideation are never identified or treated in time.
Is It Normal for New Moms to Have Intrusive Thoughts?
Intrusive thoughts, often called postpartum scary thoughts, are distressing, unwanted thoughts or mental images that suddenly pop into your mind. They might involve fears of something bad happening to your baby, images of harm, or fears about your own safety.
Here’s what’s important to understand: Intrusive thoughts are common among new mothers, and having them does not mean you want to act on them.
Research shows that up to 90% of new moms experience intrusive thoughts to some degree. These thoughts are often a symptom of postpartum anxiety or OCD, not violent intent.
They reflect the brain’s heightened state of protection and hypervigilance during early motherhood.
However, if these thoughts are persistent, cause significant distress, or are accompanied by hopelessness or thoughts of self-harm, they need immediate attention.
Intrusive thoughts often improve with therapy, rest, hormone stabilization, and targeted postpartum care. So if you’ve ever wondered, “Do intrusive thoughts go away?” — the answer is yes, with the right treatment and support, they can.
What Are the Red Flags for Postpartum Depression or Suicidal Ideation?
Many mothers hide their symptoms because they fear being judged or having their parenting questioned. But recognizing the signs, both in yourself and in those you love, can be lifesaving.
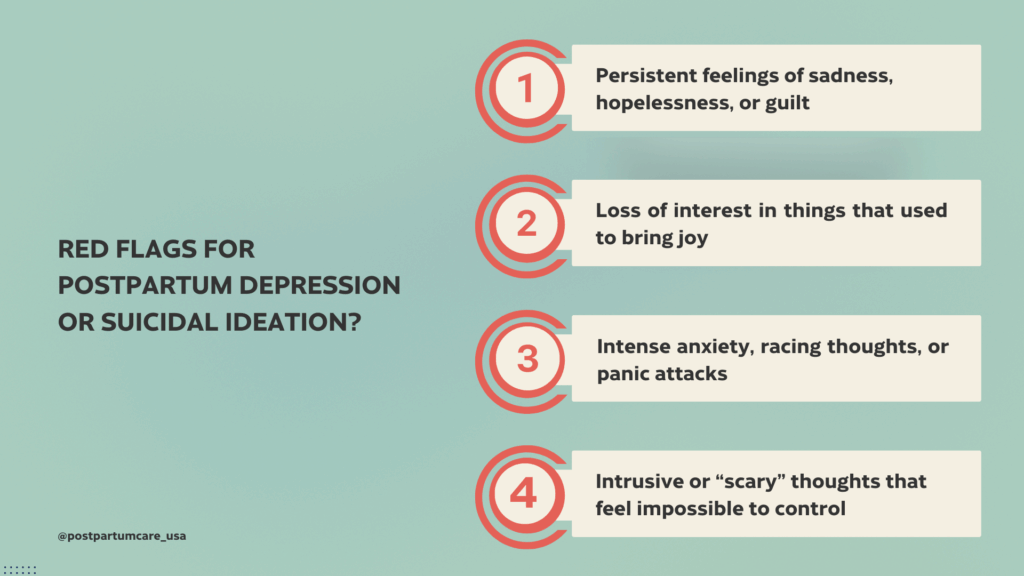
Here are key red flags to watch for:
- Persistent feelings of sadness, hopelessness, or guilt
- Loss of interest in things that used to bring joy
- Feeling disconnected from your baby or yourself
- Changes in sleep or appetite beyond normal newborn adjustment
- Intense anxiety, racing thoughts, or panic attacks
- Thoughts of harming yourself or believing your family would be “better off without you”
- Intrusive or “scary” thoughts that feel impossible to control
If any of these resonate with you, especially thoughts of self-harm or suicide, please reach out for help right now. You can call or text 988 (Suicide and Crisis Lifeline) or, if you’re outside the U.S., find international hotlines here, or go to your nearest emergency department.
Why Postpartum Suicidal Thoughts Happen
Understanding why this happens can reduce shame and open the door to healing.
After birth, a woman’s body undergoes dramatic hormonal shifts — estrogen and progesterone levels drop sharply, thyroid function changes, and neurotransmitters like serotonin fluctuate.
Combined with exhaustion, nutrient depletion, and emotional strain, this can create the perfect storm for depression and anxiety.
Beyond biology, systemic factors matter too. In the U.S., postpartum care often ends at six weeks, long before many women stabilize hormonally or emotionally. Cultural pressures to “bounce back,” lack of childcare support, and isolation all compound the risk.
The Chin et al. review also highlights that many women who die by suicide had contact with a healthcare provider in the months before their death, but were not screened for mental health symptoms. This reveals a major gap in our healthcare system — one that emphasizes physical healing immediately postpartum while overlooking emotional and psychiatric recovery in the long-term.
Postpartum Suicidal Ideation Statistics
Recent data suggests:
- Suicide accounts for 5–20% of maternal deaths in high-income countries.
- Most perinatal suicides occur within 9–12 months postpartum.
- Less than 40% of women who die by suicide during the postpartum period had contact with a mental health professional in the 30 days before their death.
These numbers highlight an urgent truth: maternal suicide is preventable, but only if we start taking postpartum mental health seriously.
What Helps with Postpartum Scary Thoughts
If you’re experiencing intrusive or suicidal thoughts, help is available — and recovery is possible. Treatment often includes:
- Comprehensive postpartum lab testing to identify hormonal or thyroid imbalances
- Therapy and support groups to address depression, anxiety, or trauma
- Medication, when appropriate, guided by a provider who understands perinatal pharmacology
- Lifestyle and nutrition support to replenish nutrients depleted during pregnancy and birth
- Community and connection, because healing rarely happens in isolation
At Postpartum Care USA, we take a whole-body approach to mental health, addressing not just the emotional symptoms, but also the biological and physiological factors that contribute to them. You deserve care that looks beyond “you’re fine” and gets to the root of what’s really going on.
You’re Not Alone
If you’ve had thoughts of not wanting to be here, or if the weight of motherhood feels unbearable, please know this:
You are not weak. You are not a bad mom. You are not alone.
These thoughts are signals of pain, not character flaws. And with the right help, they can get better.
💛 If you’re struggling, please reach out today.
You can call or text 988, or talk to your provider about a postpartum mental health evaluation.
And if you’d like to work with a team that understands both the physical and emotional sides of postpartum healing, book a call with Postpartum Care USA.
Because your life matters. Your healing matters. And you deserve to feel whole again.

Postnatal Depletion
Meet the Team
Our Services
Supplements
A virtual healthcare clinic that helps postpartum mamas recover from postnatal depletion syndrome with a holistic approach.

Get in touch