If you’re experiencing breast pain, redness, or swelling, you might be dealing with mastitis. Recognizing these symptoms early is crucial for effective treatment and faster recovery. This guide will walk you through the symptoms of mastitis and what steps to take next.
Key Takeaways
- Recognizing early symptoms of mastitis, like redness and swelling, is crucial for prompt treatment and recovery.
- Proper breastfeeding techniques and hygiene can greatly reduce the risk of developing mastitis.
- Continuing to breastfeed during mastitis is beneficial, as it helps relieve symptoms and promotes healing.
Recognizing Mastitis Symptoms
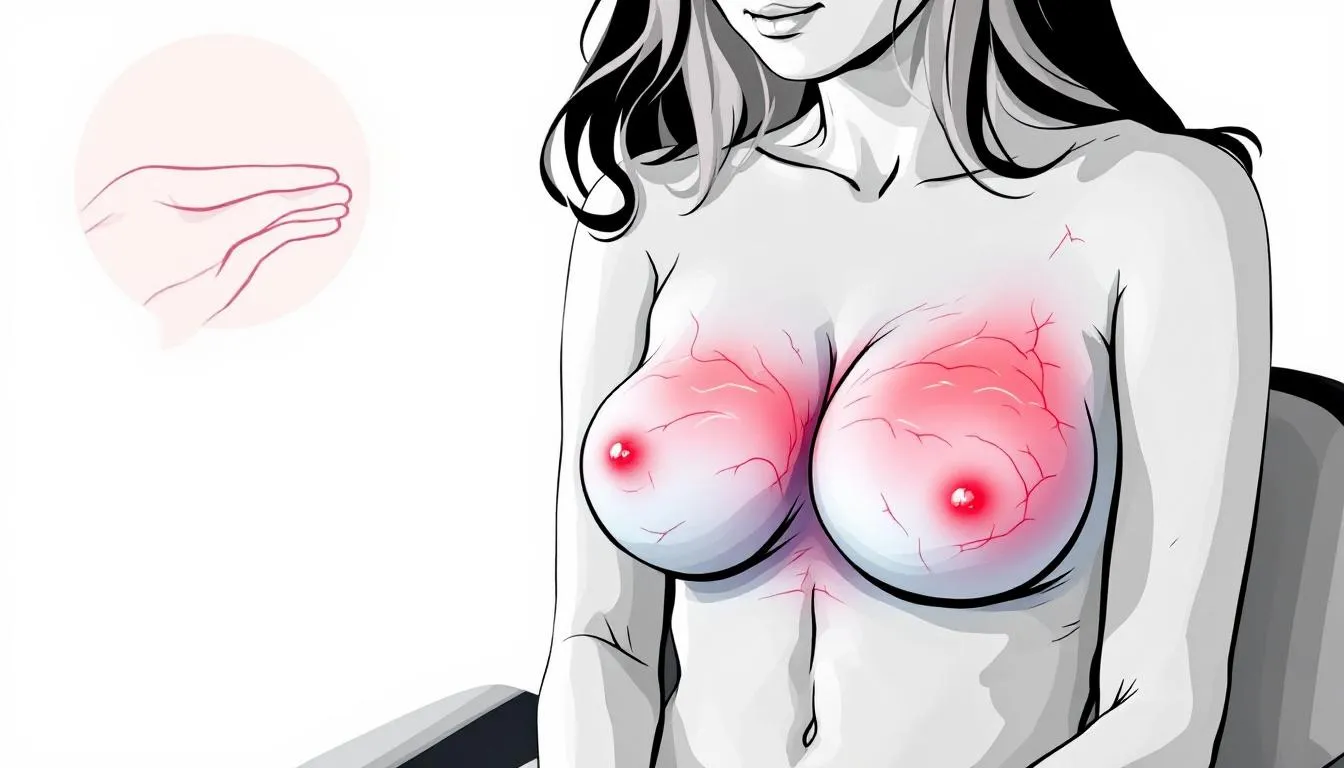
Mastitis is an inflammation of the breast tissues that can cause significant discomfort and distress, including painful inflammation and inflammatory mastitis, as well as breast inflammation. Common symptoms may involve:
- Redness
- Swelling
- Warmth
- Tenderness in the breast
Typically, these symptoms affect only one breast. The affected area often feels hard or lumpy and is painful to the touch, which can be a sign of breast lumps or breast cancer. Additionally, breast tissue in a swollen area may also indicate these conditions, including sore breasts.
Early detection of these symptoms is key to effective treatment and preventing complications. Catching it early can prevent progression to more severe symptoms and ensure a smoother recovery.
Early Signs of Mastitis
The early signs of mastitis often sneak up on you, manifesting quickly and catching many new mothers off guard. Initial symptoms can include engorgement, warmth in the affected area, and flu-like symptoms such as body aches and fatigue. These symptoms typically involve swollen and tender breasts, warmth to the touch, and significant discomfort.
Clogged milk ducts, often due to milk buildup, can lead to these initial symptoms, causing swelling and engorgement. Women in the early stages of breastfeeding, especially within the first three months, are more prone to experience these symptoms. Identifying these early signs promptly allows for timely intervention, preventing complications and promoting quicker healing.
Advanced Symptoms and Complications of a Breast Infection
If mastitis is left untreated, the symptoms can escalate rapidly. High fever and intense pain are critical signs that necessitate immediate medical care due to breast infection. Persistent high fever and significant breast pain are indicators of severe mastitis, signaling that the condition has progressed and requires urgent attention.
One of the most serious complications of untreated puerperal mastitis is the formation of an abscess, a painful collection of pus that may need surgical drainage. In extreme cases, hospital interventions might be necessary to manage bacterial mastitis effectively.
Prompt detection and treatment are essential to prevent severe outcomes.
Causes and Risk Factors for Mastitis
Mastitis can be triggered by a variety of factors, and understanding these can help in both prevention and treatment. Breastfeeding education can enhance understanding of proper techniques, potentially reducing the risk of developing mastitis. Staying hydrated and maintaining a balanced diet are important for overall breast health and can help prevent mastitis.
Avoiding sleeping positions that apply pressure to the breasts can help prevent tissue trauma that may lead to mastitis. Additionally, keeping nipples clean and dry can significantly reduce the risk of mastitis. Awareness of these factors enables proactive steps to minimize risk.
Common Causes of Mastitis
Mastitis often occurs when a breast does not completely empty during breastfeeding, leading to a clogged milk duct. Improper feeding techniques and infrequent breastfeeding can also contribute to this condition, which can cause women to develop mastitis. Ensuring proper latch and frequent feeding helps avoid milk buildup.
If you’re in need of breastfeeding support and you’re local to the Indianapolis area, we highly recommend the team at
Indy Lactation Care. Regardless, there are tons of lactation consultants and counselors that you can see virtually or in-person and many are covered by insurance. Proper feeding and breast milk elimination from the milk ducts is essential in preventing mastitis infection.
Infections can enter through the nipple due to cracks or breaks in the skin, leading to bacterial infections that cause the milk ducts to become inflamed. Initial symptoms of a mastitis infection may include tenderness, warmth, and feelings of being unwell, often resembling flu-like symptoms, and can be exacerbated by nipple damage or cracked nipples. A breast infection may also develop in these circumstances.
Proper breast feeding techniques and hygiene can help mitigate these risks.
Who is at Risk?
Certain groups are more susceptible to developing mastitis. Women who have previously experienced mastitis are at a greater risk of recurrence. Improper breastfeeding techniques significantly increase the likelihood of developing mastitis.
Breastfeeding women are the primary demographic affected by mastitis, but it’s crucial to note that mastitis affects anyone who can develop this condition if the risk factors are present. Proper breastfeeding education can significantly reduce these risks.
Prevention Strategies for Mastitis
Prevention is always better than cure, and this holds true for mastitis as well. The primary trigger for mastitis is milk that remains trapped in the breast. Factors like stress, poor nutrition, and smoking can heighten the risk of developing mastitis.
An excess supply of milk, known as hyperlactation, commonly leads to lactation mastitis. Strategies to avoid mastitis include proper latch, maintaining hygiene, and frequent breastfeeding, especially if there is too much milk supply.
Effective Breastfeeding Techniques
Frequent breastfeeding ensures thorough milk removal from the breast, which is crucial for preventing mastitis and milk duct blockages. A proper latch is crucial for effective milk transfer, preventing complications like mastitis.
Lactation consultants offer valuable lactation support and guidance for proper breastfeeding techniques, helping to correct issues with latching, positioning, and feeding frequency.
Maintaining Breast Health
Maintaining breast health involves several practices that can significantly reduce the risk of mastitis. Putting pressure through breast compression or massage before feeding can help clear blocked ducts, reducing the risk of mastitis. Regularly alternating the breast used for feeding can help prevent engorgement and maintain milk flow.
Important breastfeeding tips include:
- Alternate which breast is offered first at each feeding to promote even milk drainage.
- Avoid tight, restrictive clothing and bras to help prevent mastitis.
- Do not express more milk than your baby needs to maintain healthy breast function and ensure an adequate supply of breast milk.
For advice about what to eat and avoid eating while breastfeeding, be sure to check out our
recent blog post.Treating Mastitis Effectively
When it comes to treating mastitis, both home remedies and medical treatments play crucial roles. Continuing to breastfeed can help prevent the worsening of symptoms associated with mastitis. Consult a healthcare provider if home treatments for mastitis do not improve the condition within 24 hours.
Prompt consultation can help prevent complications such as abscess formation. Seek medical help for significant changes in breast condition to prevent complications.
At-Home Remedies
At-home remedies can be effective in managing the symptoms of mastitis. Using pain relievers such as acetaminophen or ibuprofen can assist in managing discomfort. Applying a cool cloth or ice pack can reduce swelling and pain after breastfeeding.
To manage mastitis while breastfeeding:
- Continue breastfeeding to maintain milk flow and accelerate recovery.
- Apply warm compresses before breastfeeding to ease discomfort and facilitate milk flow.
- Use a cold compress after nursing to relieve swelling and discomfort.
These combined techniques significantly alleviate pain relief and promote healing.
Medical Treatments
In some cases, medical treatments are necessary to effectively treat mastitis. Untreated mastitis can progress to a breast abscess, which may necessitate surgical intervention. In severe cases, surgical procedures may be necessary to drain an abscess when antibiotics fail to resolve the infection.
Worsening symptoms despite antibiotic treatment may indicate a serious condition, such as a breast abscess or a bacterial infection. In these instances, consulting a healthcare provider is crucial for appropriate treatment. Medical intervention prevents serious complications and ensures quicker recovery.
How Long Does Mastitis Last?
The duration of mastitis can vary depending on the severity of the condition and how quickly treatment begins. Generally, with proper treatment, symptoms of mastitis start to improve within 24 to 72 hours. Most cases of acute mastitis resolve completely within 10 to 14 days. However, if left untreated or if treatment is delayed, mastitis can persist longer and may lead to complications such as breast abscesses, which require more intensive medical intervention.
It is important to note that inflammatory mastitis, characterized by painful breast inflammation without infection, may respond well to conservative measures like rest and warm compresses, resulting in a quicker recovery. On the other hand, bacterial mastitis, caused by an infection often involving Staphylococcus aureus, typically requires a course of oral antibiotics to clear the infection effectively.
In some cases, symptoms such as breast redness, swelling, and pain may linger even after the infection has been treated. This can be due to residual inflammation or tissue healing processes. Persistent or recurrent mastitis may indicate underlying issues such as nipple trauma, clogged milk ducts, or improper breastfeeding techniques, which should be addressed with the help of a breastfeeding specialist or lactation consultant.
For optimal recovery and to prevent recurrence, continuing frequent breastfeeding or milk expression is essential to maintain milk flow and prevent milk stasis. Additionally, following proper treatment and care guidelines, including pain relief measures and breast care, supports healing and reduces symptom duration.
If mastitis symptoms do not improve within 48 to 72 hours of starting treatment, or if they worsen, it is crucial to seek medical advice promptly to reassess the condition and adjust treatment as necessary.
When to Seek Professional Help
Managing mastitis effectively relies on early detection. Treatment must follow promptly to ensure the best outcomes. If symptoms are severe, a healthcare professional may suggest a breast ultrasound to assess the condition. If mastitis symptoms persist after antibiotics, further investigation, such as a biopsy, may be necessary.
Timely professional help prevents severe complications and promotes recovery.
Warning Signs of Severe Mastitis
Severe symptoms indicating immediate medical attention for acute mastitis include high fever, intense pain, and signs of a breast abscess. If mastitis is not treated, it may lead to severe infections and could result in the formation of abscesses, necessitating surgical intervention.
Recognizing these warning signs prevents the condition from worsening.
Hospital Interventions
For persistent or severe cases, consult a healthcare provider who may prescribe antibiotics or recommend therapeutic ultrasound. In extreme cases, surgical drainage of an abscess may be necessary to treat severe mastitis effectively with appropriate treatment for mastitis, including concerns related to staphylococcus aureus.
Timely medical attention prevents serious complications.
Continuing Breastfeeding with Mastitis
Continuing to breastfeed during mastitis is generally recommended because:
- It can help alleviate symptoms.
- Stopping breastfeeding during mastitis will worsen the blockage.
- Maintaining milk flow through breastfeeding prevents blockages and promotes comfort.
Despite the discomfort, the benefits of continued breastfeeding in resolving mastitis outweigh the temporary challenges.
Benefits of Continued Breastfeeding
Maintaining milk flow through breastfeeding has several benefits:
- Prevents blockages and promotes comfort.
- Expedites infection resolution by clearing clogged ducts.
- Remains an important practice even when experiencing mastitis to improve milk flow.
Despite the discomfort, the benefits of continued breastfeeding in resolving mastitis outweigh the temporary challenges.
Tips for Managing Pain
Adequate rest aids in the recovery from mastitis. Therapeutic breast massage techniques help manage discomfort while nursing with mastitis. Frequent emptying of the affected breast prevents further blockage during mastitis.
Combining rest, therapeutic massage, and proper breast emptying techniques can significantly relieve pain while nursing.
Conclusion
Mastitis can be a challenging and painful experience, but with early recognition, proper care, and support, it is manageable and often quickly resolved. Continuing to breastfeed, practicing effective techniques, and seeking timely treatment are key to preventing complications and promoting healing. Remember, you don’t have to navigate this journey alone—professional guidance can make all the difference.
If you’re experiencing symptoms of mastitis or need support with breastfeeding and postpartum healing, book a virtual health assessment with us today. Let us help you find the care and resources you need to ensure a comfortable and successful breastfeeding experience.




Get in touch