If you’re dealing with persistent belly bloat after giving birth, you’re far from alone. That uncomfortable, distended feeling in your abdomen didn’t disappear with your baby’s arrival—and that’s completely normal for most new mothers experiencing this frustrating symptom. Bloating postpartum affects up to 80% of women in the early weeks and months following delivery, making it one of the most common postpartum complaints (Source).
While this abdominal distension can be concerning, especially when you expected your body to “bounce back” after pregnancy, understanding its causes and management strategies can provide both relief and peace of mind.
This comprehensive guide will walk you through everything you need to know about postpartum bloating, from identifying the root cause of your symptoms to implementing effective treatment options that actually work. You’ll learn when bloating is totally normal and when it might signal something requiring medical attention.
Key Takeaways
- Postpartum bloating is common and can be caused by multiple factors including diastasis recti, constipation, hormonal changes, and dietary factors
- Diastasis recti doesn’t directly cause bloating but weakens core support, making bloating more visible and pronounced
- Most postpartum bloating can be managed through core strengthening, proper nutrition, hydration, and breathing techniques
- Bloating typically appears worse in the evening and may persist for months after delivery
- Persistent or severe bloating accompanied by pain should be evaluated by a healthcare provider
What Is Postpartum Bloating?
Postpartum bloating refers to abdominal distension, a sensation of fullness, and often discomfort that develops after childbirth. Unlike the growing uterus during pregnancy that caused your belly to expand, post-pregnancy bloating stems from different mechanisms affecting your digestive tract and abdominal wall.
This condition can begin immediately after delivery and persist for weeks to months. The sensation often comes with other symptoms like excess gas, abdominal pain, and feelings of incomplete bowel movements. Many women describe feeling like they still look pregnant months after giving birth, which can be emotionally challenging during an already demanding time.
Timeline and Prevalence
Research shows that bloating postpartum affects the vast majority of new mothers, with studies indicating prevalence rates of up to 80% in the first few weeks after delivery. The intensity and duration vary significantly between individuals, with some experiencing mild discomfort that resolves within a few weeks, while others deal with more pronounced symptoms lasting several months.
Evening bloating tends to be more severe due to the accumulation of gas and fluid throughout the day, combined with weakened abdominal muscles that provide less support as fatigue sets in.
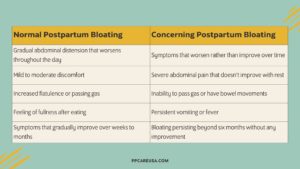
Normal vs. Concerning Symptoms
While some degree of bloating is totally normal during postpartum recovery, certain symptoms warrant immediate medical attention:
Normal postpartum bloating includes:
- Gradual abdominal distension that worsens throughout the day
- Mild to moderate discomfort
- Increased flatulence or passing gas
- Feeling of fullness after eating
- Symptoms that gradually improve over weeks to months
Concerning bloating symptoms requiring medical evaluation:
- Severe abdominal pain that doesn’t improve with rest
- Inability to pass gas or have bowel movements
- Persistent vomiting
- Fever accompanying bloating
- Symptoms that worsen rather than improve over time
- Bloating persisting beyond six months without any improvement
How Postpartum Bloating Differs from Pregnancy Bloating
During pregnancy, bloating primarily resulted from your growing uterus displacing internal organs and hormonal changes that slowed digestion. Post pregnancy, the mechanisms shift dramatically. Your uterus begins shrinking back to its pre-pregnancy size, but other factors take center stage in causing abdominal distension.
The connective tissue and abdominal muscles have been stretched and weakened, hormonal fluctuations affect digestion differently, and new lifestyle factors like irregular eating and sleeping patterns and stress from caring for a newborn contribute to digestive issues.
Primary Causes of Postpartum Bloating
Understanding the root cause of your bloating is essential for choosing the most effective management approach. Several interconnected factors typically contribute to postpartum abdominal distension.
Diastasis Recti and Core Weakness
Diastasis recti postpartum represents one of the most significant contributors to the appearance and sensation of bloating after childbirth. This condition involves the separation of the rectus abdominis muscles along the linea alba—the connective tissue running down the center of your abdomen.
During pregnancy, your abdominal muscles stretch to accommodate your growing baby. After delivery, these muscles often remain separated, creating a gap that weakens your abdominal wall’s ability to support your internal organs effectively.
How to perform a self-check for diastasis recti:
- Lie on your back with knees slightly bent and feet flat on the floor
- Place your fingers horizontally above your belly button
- Gently lift your head and shoulders off the ground
- Feel for a gap between the muscle bands
- Check how many fingers fit in the space
If two or more fingers fit in the gap, you likely have diastasis recti. While this condition doesn’t directly create excess gas or digestive issues, it significantly impacts how bloating appears and feels.
This video from Expecting and Empowered demonstrates how you can do this check on yourself but don’t hesitate to reach out to a Physical Therapist or Pelvic Floor Therapist if you think you need further evaluation.
When your abdominal muscles lack proper tone and the connective tissues remain stretched, your internal organs can push forward more easily because of abdominal separation, making any bloating much more visible and pronounced. This is why many women notice their belly bloat appears worse in the evening—as the day progresses and fatigue sets in, weakened muscles provide even less support.
The pelvic floor muscles also play a crucial role in core stability. These muscles, which support your bladder, uterus, and rectum, often become weakened or damaged during childbirth. When the pelvic floor doesn’t function optimally, it affects your body’s ability to maintain proper intra-abdominal pressure and support your digestive organs.
Digestive Issues and Constipation
Constipation ranks among the most common causes of postpartum bloating, affecting the majority of women regardless of delivery method. Multiple factors contribute to sluggish bowel movements after giving birth:
Reduced mobility and activity: Whether you delivered vaginally or via cesarean section, the first few weeks postpartum typically involve decreased physical activity. This reduction in movement slows down your digestive tract and can lead to trapped gas and harder stools.
Medication effects: Pain medications, particularly opioids prescribed after cesarean deliveries, significantly slow gut motility. Iron supplements, commonly recommended for postpartum anemia, also contribute to constipation and can cause additional bloating.
Dehydration: Blood loss during delivery, combined with the increased fluid demands of breastfeeding, can lead to dehydration. When your body doesn’t have adequate fluid, it absorbs more water from the colon, resulting in harder stools and more difficult bowel movements.
Pelvic floor damage: Vaginal deliveries, especially those involving forceps, vacuum extraction, or prolonged pushing, can damage the pelvic floor muscles and anal sphincter. This damage affects your ability to coordinate bowel movements effectively and may lead to incomplete evacuation and increased bloating.
The combination of these factors creates a cycle where constipation leads to more bloating, which can cause abdominal strain and discomfort, potentially making the problem worse.
Hormonal Changes
The dramatic hormonal shifts that occur after giving birth significantly impact your digestive system. During pregnancy, elevated levels of progesterone and estrogen affected gut motility, and the sudden drop in these hormones after delivery creates additional digestive challenges.
Estrogen and progesterone withdrawal: These hormones help regulate smooth muscle function throughout your body, including in your digestive tract. Their rapid decline after placental delivery can lead to slower peristalsis (the wave-like contractions that move food through your intestines), contributing to gas buildup and bloating.
Breastfeeding hormones: If you’re nursing, elevated prolactin levels can cause your body to retain more water, contributing to feelings of fullness and bloating. Additionally, the hormonal demands of milk production can affect your appetite and eating patterns, potentially disrupting normal digestion.
Stress hormones: The sleep deprivation and emotional demands of caring for a newborn activate your body’s stress response. Elevated cortisol levels can slow digestion, increase inflammation, and alter gut bacteria composition, all of which contribute to more bloating and digestive discomfort.
These hormonal changes typically stabilize within 6-12 months postpartum, though breastfeeding can extend the timeline for some women.
Dietary and Lifestyle Factors
The demands of new motherhood often dramatically alter eating patterns and food choices, frequently in ways that promote bloating and digestive discomfort.
Irregular eating patterns: Caring for a newborn makes maintaining regular meal times challenging. Skipping meals or eating large, infrequent portions can disrupt normal digestive rhythms and lead to increased gas production and bloating.
Trigger foods consumption: When you’re exhausted and pressed for time, it’s easy to rely on processed foods, sugary snacks, and convenience items that are more likely to cause bloating. Common culprits include:
- High-sodium processed foods that promote water retention
- Dairy products, especially if you’ve developed temporary lactose sensitivity
- Excess fructose from fruit juices and sugary foods
- Artificial sweeteners that can ferment in the gut
- Cruciferous vegetables eaten in large quantities
Inadequate hydration: Between the demands of breastfeeding and simply forgetting to drink water while caring for a baby, many new mothers become chronically dehydrated. This affects digestion and can worsen constipation and bloating.
Stress eating and emotional factors: The emotional challenges of postpartum recovery, combined with sleep deprivation, can lead to stress eating or choosing comfort foods that may not agree with your digestive system.
Effective Management Strategies
Successfully managing bloating postpartum requires a multi-faceted approach that addresses the underlying causes while providing symptomatic relief. The following strategies have proven most effective for reducing both the appearance and discomfort of postpartum abdominal distension.
Core Strengthening and Breathing Techniques
Rebuilding strength in your abdominal muscles and pelvic floor represents the foundation of long-term bloating management, especially when diastasis recti contributes to your symptoms.
Safe postpartum exercises to start with:
Diaphragmatic breathing: This fundamental exercise helps re-coordinate your core muscles while providing gentle massage to your internal organs, promoting better digestion and gas movement.
- Lie comfortably with knees slightly bent and feet flat
- Place one hand on your chest, one on your belly
- Breathe slowly through your nose, allowing only your belly to rise
- Exhale slowly through pursed lips, gently drawing your belly button toward your spine
- Practice for 5-10 minutes several times daily
Pelvic tilts: These gentle movements help re-engage your deep abdominal muscles without creating abdominal strain.
- Lie on your back with knees bent and feet flat
- Gently tilt your pelvis, pressing your lower back toward the floor
- Hold for 5 seconds, then release
- Repeat 10-15 times, focusing on controlled movement
Modified bridges: This exercise strengthens your glutes and core while being safe for postpartum recovery.
- Lie on your back with knees bent
- Squeeze your glutes and lift your hips, creating a straight line from knees to shoulders
- Hold for 3-5 seconds, then lower slowly
- Start with 10 repetitions, gradually increasing as strength improves
Wall sits: These provide core activation without putting stress on healing abdominal muscles.
Important exercises to avoid: Traditional sit ups and crunches should be avoided, especially if you have diastasis recti, as they can worsen abdominal separation and increase intra-abdominal pressure without effectively addressing the underlying muscle weakness.
Pelvic floor exercises (kegel exercises):
Proper pelvic floor function is essential for core stability and digestive health. Many women find that kegel exercises not only help with incontinence issues but also reduce feelings of pelvic pressure and bloating.
- Identify the right muscles by stopping urination midstream
- Contract these muscles for 3 seconds, then relax for 3 seconds
- Work up to 10-second holds
- Aim for 3 sets of 10 repetitions daily
- Ensure you’re not holding your breath or tensing other muscles
Nutritional Approaches
Strategic dietary modifications can significantly reduce bloating while supporting your body’s healing and energy needs during this demanding time.
Anti-bloating foods to emphasize:
- Asparagus: Contains natural diuretics that help reduce water retention
- Pineapple: Rich in digestive enzymes that aid protein breakdown
- Cucumber: High water content helps with hydration and reduces sodium-related bloating
- Leafy greens: Provide fiber and nutrients without causing excessive gas
- Ginger: Natural anti-inflammatory that soothes the digestive tract
Adequate fiber intake: Most women need 25-30 grams of fiber daily from sources like:
- Whole grains such as quinoa, brown rice, and oats
- Fruits like berries, apples, and pears
- Vegetables including carrots, sweet potatoes, and broccoli
- Legumes in moderate portions
The elimination diet approach:
If you suspect certain foods are triggering your bloating, consider a structured elimination approach:
- Remove potential triggers for 2-3 weeks: dairy products, gluten, processed foods, artificial sweeteners, and high-FODMAP foods
- Keep a detailed food and symptom diary
- Gradually reintroduce foods one at a time, noting any symptom changes
- Identify and avoid your personal trigger foods
Meal timing strategies:
- Eat smaller, more frequent meals rather than three large ones
- Chew food thoroughly and eat slowly to reduce air swallowing
- Avoid drinking large amounts of liquid with meals
- Allow 2-3 hours between eating and lying down
Hydration and Lifestyle Modifications
Proper hydration and lifestyle adjustments provide significant relief from bloating while supporting overall postpartum recovery.
Daily water intake recommendations:
- Base requirement: 8-10 glasses (64-80 ounces) of water daily
- Breastfeeding mothers need an additional 16-32 ounces
- Monitor urine color—pale yellow indicates adequate hydration
- Include water-rich foods like fruits and vegetables in your count
Beneficial herbal teas:
Several herbal teas can provide relief from bloating and digestive discomfort:
- Ginger tea: Reduces inflammation and promotes gastric emptying
- Peppermint tea: Relaxes digestive muscles and reduces gas
- Fennel tea: Traditional remedy for gas and bloating
- Chamomile tea: Soothes the digestive tract and promotes relaxation
Note: Always check with your healthcare provider about herbal tea safety while breastfeeding.
Posture improvement techniques:
Poor posture, common when caring for a newborn, can worsen the appearance of bloating and reduce core muscle effectiveness:
- When feeding your baby, use supportive pillows to maintain good alignment
- Take frequent breaks from hunched positions
- Practice gentle stretches throughout the day
- Consider a supportive postpartum belly wrap for additional core support during activities
Optimizing elimination:
Using a toilet stool (like a Squatty Potty) can improve the angle for bowel movements, making elimination more complete and reducing gas trapped in the colon. This simple modification can significantly reduce bloating for many women dealing with postpartum constipation.
When to Seek Medical Help
While bloating postpartum is usually a normal part of recovery, certain symptoms and situations require professional medical evaluation to rule out serious complications.
Red Flag Symptoms
Contact your healthcare provider immediately if you experience:
Severe or worsening abdominal pain: Pain that is intense, doesn’t improve with rest, or gets progressively worse may indicate complications such as:
- Bowel obstruction
- Hernia
- Infection
- Ovarian torsion or cysts
Inability to pass gas or stool: Complete inability to have bowel movements or pass gas for more than 24-48 hours can signal bowel obstruction, which requires emergency treatment.
Persistent vomiting: Ongoing nausea and vomiting, especially when accompanied by bloating, may indicate obstruction or other serious conditions.
Signs of infection: Fever, chills, or foul-smelling vaginal discharge combined with abdominal bloating could indicate postpartum infections requiring prompt medical treatment.
Visible hernias: A bulge in your abdominal wall that becomes more prominent when coughing, straining, or standing may represent an incisional hernia (after C-section) or other types of hernias requiring surgical evaluation.
Persistent Symptoms
Even without emergency symptoms, you should schedule a medical evaluation if:
- Bloating persists beyond six months without any improvement
- Symptoms are interfering significantly with daily activities or quality of life
- You’re unable to exercise or perform normal activities due to abdominal discomfort
- Bloating is accompanied by unintentional weight loss or gain weight unexpectedly
- You develop new symptoms like blood in stool or severe cramping
Specialized Conditions Requiring Treatment
Severe diastasis recti: If your abdominal separation is more than three finger-widths wide, doesn’t improve with exercise, or causes functional problems, you may need specialized physical therapy or, in severe cases, surgical intervention.
Pelvic floor dysfunction: Persistent problems with bowel or bladder control, pelvic pressure, or difficulty with evacuation may indicate significant pelvic floor damage requiring specialized treatment.
Digestive disorders: Conditions like ulcerative colitis or other inflammatory bowel diseases can sometimes develop or worsen postpartum and require specific medical treatment beyond general bloating management.
Professional Treatment Options
When self-management strategies aren’t providing adequate relief, several professional treatment options can address the underlying causes of persistent bloating postpartum.
Physical Therapy
Specialized postpartum physical therapy has become increasingly recognized as an effective treatment for both diastasis recti and pelvic floor dysfunction.
Core rehabilitation programs: Physical therapists trained in postpartum recovery can assess your specific muscle imbalances and develop targeted exercise programs. These typically include:
- Progressive abdominal strengthening that’s safe for diastasis recti
- Functional movement training for daily activities
- Breathing pattern correction
- Posture education and workplace ergonomics
Pelvic floor rehabilitation: For women with pelvic floor damage or dysfunction, specialized pelvic floor physical therapy can provide significant improvement in symptoms. Treatment may include:
- Internal assessment and treatment techniques
- Biofeedback training to improve muscle coordination
- Electrical stimulation for muscle re-education
- Education about proper toileting posture and techniques
Nutritionist Consultation
Working with a registered dietitian who understands postpartum nutrition needs can help identify trigger foods and develop sustainable eating plans that reduce bloating while meeting the demands of breastfeeding and recovery.
Personalized dietary assessment: A nutritionist can analyze your current diet, identify problematic patterns, and suggest modifications that fit your lifestyle and preferences.
Gut health optimization: Some practitioners specialize in using probiotics, prebiotics, and specific dietary approaches to restore healthy gut bacteria balance, which can significantly impact bloating and digestive comfort.
Medical Evaluation and Treatment
Diagnostic testing: If symptoms persist or are severe, your healthcare provider may recommend:
- Blood tests to check for thyroid dysfunction or other hormonal imbalances
- Imaging studies to rule out structural problems
- Stool tests to identify bacterial imbalances or infections
Medication options: In some cases, temporary use of medications may be helpful:
- Prescription-strength probiotics
- Medications to improve gut motility
- Treatment for underlying conditions like thyroid dysfunction
Surgical Options
For severe cases of diastasis recti that don’t respond to conservative treatment, surgical repair may be considered.
Diastasis recti surgery (tummy tuck with muscle repair): This procedure, technically called an abdominoplasty with rectus plication, involves:
- Surgical repair of the separated abdominal muscles
- Removal of excess skin if present
- Restoration of proper abdominal wall function
Surgery is typically reserved for cases where:
- The separation is very wide (>3-4 finger widths)
- Conservative treatment has been tried for at least 12 months
- The condition significantly impacts quality of life or function
- The patient has completed childbearing
Recovery Timeline
Most women see significant improvement in bloating symptoms within 3-6 months of starting appropriate treatment, though individual recovery timelines vary based on:
- Severity of underlying issues
- Consistency with treatment recommendations
- Overall health and other factors
- Whether surgical intervention is needed
Prevention and Long-term Management
While some degree of postpartum bloating is unavoidable, several strategies can minimize its severity and duration while promoting long-term digestive and core health.
Gradual Return to Exercise
Once you receive clearance from your healthcare provider (typically 6-8 weeks postpartum), gradually increasing physical activity provides multiple benefits for bloating management:
Start slowly: Begin with gentle walking and basic breathing exercises before progressing to more challenging activities.
Focus on functional movements: Prioritize exercises that mimic daily activities and help restore normal movement patterns:
- Squats with proper form
- Modified lunges
- Carrying exercises that engage the core
- Stairs climbing when comfortable
Avoid high-impact activities initially: Activities like running or jumping should be delayed until your core and pelvic floor have recovered adequate strength and coordination.
Listen to your body: Increase activity gradually, and don’t push through pain or significant discomfort. Some muscle fatigue is normal, but sharp pain or worsening symptoms indicate you need to slow down.
Building Sustainable Habits
Sleep optimization: While getting adequate sleep with a newborn is challenging, prioritizing rest when possible supports hormonal recovery and digestive health:
- Sleep when your baby sleeps, even during the day
- Ask for help with nighttime feedings when possible
- Create a relaxing bedtime routine
- Consider safe co-sleeping arrangements if they improve everyone’s sleep
Stress management techniques: Chronic stress significantly impacts digestion and can worsen bloating:
- Practice deep breathing exercises throughout the day
- Try gentle yoga or stretching
- Consider meditation apps designed for busy parents
- Connect with other new mothers for emotional support
- Don’t hesitate to ask for help with household tasks
Meal planning and preparation: Preparing healthy meals in advance can help you maintain good nutrition even during demanding days:
- Batch cook easy-to-digest meals on weekends
- Keep healthy snacks readily available
- Prepare smoothies with anti-bloating ingredients
- Use a slow cooker for hands-off meal preparation
Long-term Digestive Health
Maintaining adequate fiber intake: As your life settles into new routines, continue prioritizing fiber-rich foods that support regular bowel movements and healthy gut bacteria.
Staying hydrated: Make drinking water a habit by:
- Keeping a water bottle with you during feedings
- Setting phone reminders to drink water
- Eating water-rich foods like fruits and vegetables
- Monitoring your urine color as a hydration indicator
Regular movement: Even light, consistent activity helps maintain digestive health:
- Take daily walks with your baby
- Do gentle stretches during baby’s playtime
- Use stairs instead of elevators when possible
- Park farther away to increase walking
Follow-up Care
Regular healthcare checkups: Maintain consistent contact with your healthcare providers throughout your first year postpartum:
- Attend all scheduled postpartum visits
- Don’t hesitate to schedule additional appointments if symptoms concern you
- Keep track of symptoms in a journal to share with providers
- Ask questions about any changes you notice
Monitoring for improvement: Track your symptoms to identify patterns and measure progress:
- Note which foods seem to trigger bloating
- Record how different activities affect your symptoms
- Monitor your energy levels and mood
- Celebrate small improvements in strength and function
FAQ
How long does postpartum bloating typically last?
Most women see significant improvement in bloating symptoms within 3-6 months postpartum. However, the timeline varies considerably based on individual factors like the severity of diastasis recti, breastfeeding status, and how consistently you implement management strategies. Some women may experience mild symptoms for up to a year, while others see improvement within just a few weeks.
Is it normal to look pregnant months after delivery?
Yes, it’s totally normal to appear pregnant for several months after giving birth, especially if you have diastasis recti. The combination of stretched abdominal muscles, weakened connective tissue, and possible excess abdominal fat can create a persistent “pregnant” appearance. This typically improves gradually with appropriate core strengthening exercises and time.
Can breastfeeding cause bloating?
Breastfeeding can contribute to bloating through several mechanisms. The hormonal changes associated with milk production can affect digestion and cause water retention. Additionally, increased caloric needs may lead to changes in eating patterns that promote bloating. However, breastfeeding also has many health benefits, and any associated bloating usually improves as your body adjusts.
What foods should I avoid to reduce postpartum bloating?
Common trigger foods include processed foods high in sodium, excess dairy products (especially if you have temporary lactose sensitivity), artificial sweeteners, carbonated beverages, and large amounts of cruciferous vegetables like broccoli and cabbage. However, trigger foods vary between individuals, so keeping a food diary can help identify your personal problem foods.
When can I start doing ab exercises after delivery?
You should wait for clearance from your healthcare provider before starting any abdominal exercises, typically around 6-8 weeks postpartum. If you have diastasis recti, traditional ab exercises like sit ups and crunches should be avoided as they can worsen the separation. Focus instead on gentle core activation exercises and consider working with a physical therapist who specializes in postpartum recovery.
Does postpartum bloating affect future pregnancies?
Postpartum bloating itself doesn’t typically impact subsequent pregnancies. However, unresolved diastasis recti or pelvic floor weakness can contribute to similar or more severe symptoms in future pregnancies. Addressing these issues thoroughly during your current recovery can actually improve your experience in subsequent pregnancies and deliveries.
Remember that bloating postpartum, while uncomfortable and sometimes distressing, is a common part of the recovery process for most new mothers. Your body has just accomplished the incredible feat of giving birth, and it needs time to heal and readjust. Be patient with yourself, implement the strategies that work best for your situation, and don’t hesitate to seek professional help when you need it.
With the right approach combining core strengthening, proper nutrition, adequate hydration, and appropriate medical support when needed, most women can successfully manage their postpartum bloating and return to feeling comfortable and confident in their bodies. Focus on gradual, sustainable changes rather than quick fixes, and celebrate the small improvements along the way.
And if you’re interested in meeting with our providers to come up with a customized exercise and nutrition plan to combat your post pregnancy bloating and distension, you can book a call with us or visit our services page for more information.
Pin This for Later:

Postnatal Depletion
Meet the Team
Our Services
Supplements
A virtual healthcare clinic that helps postpartum mamas recover from postnatal depletion syndrome with a holistic approach.

Get in touch