Many women with polycystic ovary syndrome hope that pregnancy will provide lasting relief from their symptoms. Unfortunately, PCOS is a chronic condition that persists throughout life, often returning with renewed intensity during the postpartum period. While the temporary hormonal changes of pregnancy may mask symptoms, the reality is that women with pcos face unique challenges after delivery that require specialized attention and care.
The postpartum period brings significant hormonal fluctuations that can worsen insulin resistance, trigger cardiovascular complications, and increase the risk of mental health challenges. Understanding these risks and implementing proper management strategies is crucial for both you and your child’s long-term health outcomes.
Key Takeaways
- PCOS symptoms may temporarily improve during pregnancy but often return or worsen postpartum due to hormonal changes
- Women with PCOS face increased risk of postpartum cardiovascular complications including preeclampsia, cardiomyopathy, and thrombotic disease
- Postpartum depression and anxiety rates are 1.76 times higher in women with PCOS compared to those without the condition
- Breastfeeding challenges are common due to hormonal imbalances and insulin resistance affecting milk production
- Early screening, monitoring, and targeted interventions are essential for managing PCOS postpartum complications
- Lifestyle modifications including diet, exercise, and stress management remain crucial for symptom control after delivery
What Happens to PCOS Symptoms After Pregnancy
Polycystic ovary syndrome is a chronic endocrine disorder that affects approximately 1 in 10 women of reproductive age worldwide. During pregnancy, elevated levels of estrogen and progesterone temporarily suppress male hormones (androgens), leading many women to experience significant improvement in classic PCOS symptoms like excess hair growth, acne, and irregular periods.
However, this relief is temporary. After delivery, the dramatic decline in pregnancy hormones, combined with the onset of lactation and related shifts in reproductive hormones, typically results in the return or even worsening of PCOS manifestations.
The Hormonal Roller Coaster
The postpartum period creates a perfect storm of hormonal changes that can intensify PCOS symptoms:
- Plummeting estrogen and progesterone allow androgens to reassert their dominance
- Rising prolactin levels from breastfeeding can suppress ovulation and disrupt follicle stimulating hormone balance
- Increased cortisol from sleep deprivation and stress exacerbates insulin resistance
- Disrupted circadian rhythms from newborn care affect hormone production
Timeline of Symptom Return
The return of PCOS symptoms varies significantly among individuals:
- Some women notice changes within weeks of delivery
- Others may not experience symptom recurrence until after weaning
- Weight gain and metabolic changes often begin immediately postpartum
- Irregular periods may not resume until breastfeeding decreases or stops entirely
Research suggests that women with more severe PCOS symptoms before pregnancy tend to experience more pronounced symptom return during the postpartum period.
Postpartum Cardiovascular Complications in PCOS
Women with polycystic ovary syndrome face significantly elevated cardiovascular risks during the postpartum period compared to women without the condition. These pregnancy complications can have serious implications for both immediate and long-term health.
Increased Risk of Preeclampsia and Eclampsia
Postpartum preeclampsia affects women with PCOS at rates 1.5 to 2 times higher than the general population (Source). This dangerous condition, characterized by high blood pressure and protein in the urine, can develop up to six weeks after delivery. Warning signs include:
- Severe headaches
- Vision changes or sensitivity to light
- Upper abdominal pain
- Sudden swelling of face, hands, or feet
- Decreased urination
Peripartum Cardiomyopathy
This rare but serious heart condition occurs from one month before to five months after delivery. Women with PCOS, particularly those who are not obese, show higher rates of peripartum cardiomyopathy. Symptoms include:
- Shortness of breath
- Fatigue
- Swelling in legs, ankles, or feet
- Irregular heartbeat
- Chest pain
Thrombotic Disease and Stroke Risk
The combination of PCOS-related inflammation, insulin resistance, and postpartum hypercoagulability creates an increased risk for:
- Deep vein thrombosis
- Pulmonary embolism
- Cerebrovascular accidents (strokes)
- Congestive heart failure
A population based cohort study found that women with PCOS had significantly higher rates of these complications within the first postpartum year, emphasizing the need for vigilant cardiovascular monitoring.
Mental Health Challenges After Delivery
The mental health implications of PCOS postpartum are significant and often unrecognized. Women with polycystic ovary syndrome face substantially higher rates of postpartum depression and anxiety compared to women without the condition.
Postpartum Depression Statistics
Research reveals concerning trends in postpartum depression symptoms among women with PCOS (Source):
- 12-13.6% of women with PCOS develop postpartum depression
- 9.5-10.2% of women without PCOS experience postpartum depression
- 1.76 times higher risk ratio for women with PCOS
Contributing Factors
Several factors contribute to increased mental health risks:
- Prenatal Mental Health: Existing depression and anxiety during pregnancy account for 20-32% of the increased postpartum depression risk in women with PCOS.
- Hormonal Fluctuations: The dramatic shifts in reproductive hormones, combined with disrupted insulin levels, can trigger mood disorders even in women with no prior mental health history.
- Body Image Concerns: Postpartum weight retention, combined with returning symptoms like excess facial hair growth and thinning hair, can significantly impact self-esteem.
- Breastfeeding Challenges: Difficulties with milk production and low milk supply can create feelings of inadequacy and failure.
Early Screening and Intervention
Healthcare providers should implement proactive mental health screening for women with PCOS, beginning during pregnancy and continuing throughout the postpartum period. Both depressed mood and anhedonia (loss of interest in activities) are significantly more prevalent in this population.
Breastfeeding Challenges with PCOS
Many women with polycystic ovary syndrome encounter significant obstacles when attempting to breastfeed their newborns. These challenges stem primarily from the hormonal imbalances and metabolic dysfunction characteristic of the condition.
Delayed Milk Production
One of the most common issues is delayed lactogenesis, where milk coming in is postponed by 24-48 hours or more after birth. This delay occurs because:
- High androgen levels interfere with mammary gland development
- Insulin resistance affects the energy metabolism required for milk production
- Elevated body mass index, common in PCOS, compounds lactation difficulties
Reduced Milk Supply
Even when milk production begins, maintaining adequate supply can be challenging. The exact cause involves multiple factors:
- Insufficient glandular tissue: Some women with PCOS have underdeveloped breast tissue due to hormonal disruptions during puberty
- Metabolic interference: High insulin levels disrupt the normal fat-burning processes needed for efficient breast milk production
- Hormonal competition: Elevated androgens may compete with prolactin’s milk-producing effects
Individual Variation in Breastfeeding Success
It’s important to note that not all women with PCOS experience breastfeeding difficulties. Many successfully establish and maintain healthy milk supply with proper support. Individual assessment by a lactation consultant is crucial for determining the best approach for each mother.
Managing Insulin Resistance During Breastfeeding
Elevated insulin levels postpartum can create a cascade of problems affecting both milk supply and maternal health:
Impact on Milk Production: High insulin interferes with the body’s ability to burn fat efficiently, which is essential for energy during lactation. This metabolic disruption can lead to:
- Inconsistent milk supply
- Altered breast milk composition
- Increased difficulty losing pregnancy weight
Therapeutic Approaches: Many healthcare providers recommend continuing metformin during breastfeeding under medical supervision. This medication can help:
- Stabilize insulin levels
- Support consistent milk production
- Improve maternal metabolic health
- Benefit infant health through improved milk quality
Postpartum PCOS Management Strategies
Effective management of PCOS postpartum requires a comprehensive, multidisciplinary approach that addresses the complex interplay of hormonal, metabolic, and psychological factors.
Medical Management
Metformin Continuation
Most healthcare providers recommend continuing metformin therapy during the postpartum period and breastfeeding. This medication helps:
- Control blood sugar levels
- Reduce insulin resistance
- Support weight management
- Potentially improve milk supply
Blood Pressure Monitoring
Given the increased risk of postpartum preeclampsia and hypertensive heart disease, regular blood pressure monitoring is essential. This includes:
- Daily home monitoring for the first few weeks
- Weekly healthcare provider checks for the first month
- Monthly monitoring for the first six months
Cardiovascular Assessment
Women with PCOS should receive more frequent cardiovascular evaluations, including:
- EKG screening within the first postpartum month
- Echocardiogram if symptoms of heart dysfunction appear
- Lipid panel and diabetes screening at 6-12 weeks postpartum
Lifestyle Modifications for Symptom Control
Nutritional Approach: A heart-healthy diet focusing on managing insulin resistance includes:
- Complex carbohydrates with low glycemic index
- Lean proteins at every meal
- Healthy fats from sources like avocados, nuts, and olive oil
- Regular meal timing to stabilize blood sugar
- Adequate hydration to support milk production
Exercise Implementation: Physical activity should be gradually reintroduced after medical clearance:
- Walking as soon as comfortable after delivery
- Strength training to improve insulin sensitivity
- Cardiovascular exercise for heart health
- Flexibility and stress-reduction activities like yoga
Sleep Optimization: Despite the challenges of newborn care, prioritizing sleep is crucial:
- Napping when the baby sleeps
- Creating a consistent bedtime routine
- Managing stress through relaxation techniques
- Seeking help with nighttime feeding when possible
Stress Management: Chronic stress worsens insulin resistance and can trigger mood disorders:
- Mindfulness meditation
- Deep breathing exercises
- Connecting with support groups for new mothers
- Professional counseling when needed
When to Seek Medical Attention When You Have PCOS Postpartum
Recognizing warning signs and knowing when to seek immediate medical attention can be life-saving for women with PCOS postpartum.
Cardiovascular Emergency Signs
Contact emergency services immediately for:
- Severe headaches accompanied by vision changes or confusion
- Chest pain or pressure, especially with shortness of breath
- Sudden swelling of face, hands, or feet
- Upper abdominal pain that doesn’t resolve
- Difficulty breathing or feeling like you can’t catch your breath
Mental Health Urgent Concerns
Seek immediate psychiatric evaluation for:
- Thoughts of harming yourself or your baby
- Persistent depressed mood lasting more than two weeks
- Inability to care for yourself or your infant
- Severe anxiety or panic attacks
- Hearing voices or seeing things that aren’t there
Metabolic and Hormonal Red Flags
Schedule urgent medical evaluation for:
- Uncontrolled weight gain (more than 2-3 pounds per week)
- Signs of diabetes: excessive thirst, frequent urination, blurred vision
- Significant changes in milk supply or sudden cessation
- Severe fatigue that doesn’t improve with rest
- New or worsening symptoms like excess facial hair or severe acne
Breastfeeding Complications
Consult a lactation specialist or healthcare provider for:
- No milk production by day 5 postpartum
- Sudden decrease in milk supply
- Severe breast pain or signs of infection
- Baby showing signs of dehydration or poor weight gain
Long-term Health Considerations for Women with Polycystic Ovarian Syndrome
Polycystic ovary syndrome creates lifelong health implications that extend far beyond the immediate postpartum period. Understanding these long-term risks is essential for developing effective prevention strategies.
Cardiovascular Disease Risk
Women with PCOS face significantly elevated lifetime risks of:
- Hypertension: Up to 40% will develop high blood pressure
- Type 2 diabetes: Risk increases 4-7 times compared to women without PCOS
- Heart disease: Earlier onset and more severe presentations
- Stroke: Increased risk beginning in the fourth decade of life
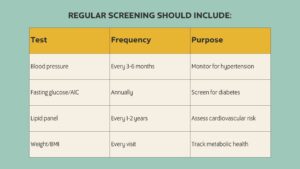
Metabolic Monitoring Schedule
Regular screening should include the following.
Impact on Child Health
Children born to mothers with PCOS face increased risks that warrant ongoing monitoring:
Childhood Obesity: Research suggests higher rates of obesity in children of mothers with PCOS, likely due to both genetic factors and intrauterine environmental influences.
Metabolic Dysfunction: These children may develop insulin resistance and metabolic syndrome at younger ages, emphasizing the importance of family-wide healthy lifestyle interventions.
Reproductive Health: Daughters may have higher rates of PCOS, while sons may face increased risk of metabolic disorders.
Family-Centered Health Approach
Implementing lifestyle changes that benefit the entire family includes:
- Preparing nutritious meals that support healthy metabolism
- Engaging in regular physical activity as a family
- Establishing consistent sleep routines for all family members
- Teaching children about healthy eating and body image
Future Pregnancy Planning
Women with PCOS who plan additional pregnancies should consider:
- Achieving optimal weight before conception
- Managing insulin resistance and blood pressure
- Genetic counseling if there’s family history of metabolic disorders
- Preconception mental health support
The national institutes of health and american college of obstetrics and gynecology recommend specialized preconception care for women with PCOS to optimize postpartum outcomes.
Building Your Support Team
Managing PCOS postpartum effectively requires a coordinated team of healthcare professionals, each bringing specialized expertise to address the complex challenges of this condition.
Essential Healthcare Providers
Primary Care Physician: Your healthcare provider serves as the central coordinator of your care, managing routine screening, medication adjustments, and referrals to specialists as needed.
Endocrinologist: Specializes in hormonal disorders and can provide expert management of insulin resistance, diabetes prevention, and complex hormonal imbalances that affect both you and your ability to manage PCOS symptoms effectively.
Cardiologist: Given the significantly increased cardiovascular risks, women with PCOS may benefit from specialized cardiac care, particularly if they develop high blood pressure, heart disease, or other cardiovascular complications.
Mental Health Professional: A psychiatrist or psychologist with experience in perinatal mood disorders can provide crucial support for managing postpartum depression symptoms, anxiety, and the psychological challenges of living with a chronic condition.
Lactation Consultant: If you choose to breastfeed, working with a certified lactation consultant can help address the unique challenges faced by women with PCOS, including delayed milk production and maintaining adequate milk supply.
Registered Dietitian: A nutrition specialist can help develop personalized meal plans that address insulin resistance, support healthy weight management, and optimize nutrition for both maternal health and milk production.
Building Your Personal Support Network
Beyond medical professionals, personal support is equally important:
- Family and friends who understand your condition and can provide practical help with childcare and household tasks
- Support groups for women with PCOS or new mothers facing similar challenges
- Online communities that provide 24/7 access to others who understand your experiences
- Childcare assistance that allows you to attend medical appointments and engage in self-care activities
Frequently Asked Questions About PCOS
Does PCOS go away after having a baby? No, polycystic ovary syndrome is a chronic condition that does not disappear after pregnancy. While symptoms may improve temporarily during pregnancy due to hormonal changes, they typically return postpartum and require ongoing management throughout life.
How long do postpartum PCOS symptoms last? Postpartum PCOS symptoms can persist indefinitely, as PCOS is a lifelong condition. However, with proper management including lifestyle modifications, medical treatment, and regular monitoring, the severity and impact of symptoms can be significantly reduced.
Can I continue taking metformin while breastfeeding? Many women safely continue metformin during breastfeeding under medical supervision. Only small amounts transfer to breast milk, and the benefits for managing insulin resistance often outweigh the minimal risks. Always consult your healthcare provider about medication safety during lactation.
Why is my PCOS worse after pregnancy? Several factors can worsen PCOS symptoms postpartum, including dramatic hormonal fluctuations, increased insulin resistance from weight gain and stress, sleep deprivation affecting hormone production, and the metabolic demands of breastfeeding. These factors can increase both insulin levels and male hormones.
When should I resume PCOS treatment after delivery? PCOS management should typically begin immediately postpartum with guidance from your healthcare team. Early intervention helps prevent complications, supports successful breastfeeding if desired, and reduces the risk of long-term health problems. Don’t wait for symptoms to worsen before seeking treatment.
Can PCOS affect my ability to lose pregnancy weight? Yes, insulin resistance and metabolic changes associated with PCOS can make postpartum weight loss more challenging. The condition affects how your body processes carbohydrates and stores fat, making a structured approach with medical support, proper nutrition, and regular exercise essential for achieving healthy weight loss goals.
Conclusion
The postpartum period represents a critical window for women with polycystic ovary syndrome, requiring vigilant monitoring and proactive management to prevent serious complications. While the challenges are significant—from increased cardiovascular risks to mental health concerns and breastfeeding difficulties—understanding these risks empowers you to take control of your health journey.
The key to successful PCOS postpartum management lies in early recognition that this chronic condition requires lifelong attention, not just during pregnancy. By working closely with a multidisciplinary healthcare team, implementing evidence-based lifestyle modifications, and maintaining regular monitoring for both immediate and long-term health risks, women with PCOS can navigate the postpartum period safely and optimize their health for years to come.
Remember that managing PCOS postpartum is not just about your own health—it’s also about creating the foundation for your child’s future wellbeing and your family’s overall health. Take an active role in your care, advocate for the support you need, and don’t hesitate to seek help when concerns arise. Your proactive approach to managing PCOS during this vulnerable period will pay dividends for both your immediate recovery and your long-term women’s health outcomes.
Pin This for Later:

Postnatal Depletion
Meet the Team
Our Services
Supplements
A virtual healthcare clinic that helps postpartum mamas recover from postnatal depletion syndrome with a holistic approach.

Get in touch