Postpartum preeclampsia isn’t just rare—it’s dangerously overlooked.
In 2022, just five days after giving birth, my friend Chelsea reached out to me complaining of severely swollen legs and a high blood pressure reading of 165/100. Within hours, she was fighting for her life in the ICU, diagnosed with peripartum cardiomyopathy following severe postpartum preeclampsia.
What happened next was terrifying. Within 12 hours, Chelsea had coded, was intubated, and was life-lined to an ICU where she was diagnosed with peripartum cardiomyopathy. She spent a week in critical care and only survived because she sought help in time.
This is the reality of postpartum preeclampsia—a condition most women have never even heard of until it’s nearly too late.
Her story is a powerful reminder: signs like swelling, headaches, and high blood pressure after birth are not normal. They are medical red flags that demand immediate attention.
In this post, we’ll walk through:
- what preeclampsia postpartum is
- why it happens and what risk factors make women more prone to developing postpartum preeclampsia
- how long postpartum preeclampsia can last, and
- how to treat postpartum preeclampsia
We’ll provide answers to common questions like “Does postpartum preeclampsia go away?” and “How serious is postpartum preeclampsia?”
Chelsea’s story could have ended in tragedy, but thanks to early recognition and action, she’s now home with her husband and son. Let her survival be your warning—and your call to action.
What Is Postpartum Preeclampsia?
Postpartum preeclampsia, also known as postpartum toxemia, is a potentially life-threatening condition that occurs when a woman develops high blood pressure and signs of organ stress after giving birth—most commonly within the first 48 hours, but it can appear up to six weeks or even later in rare cases (Source).
Unlike typical preeclampsia during pregnancy, postpartum preeclampsia can catch women off guard because symptoms arise after delivery, when many assume the risk has passed.
What Causes Postpartum Preeclampsia?
The exact cause is still unknown, but researchers believe it may be triggered by a combination of factors such as:
- Damage to the blood vessels
- Immune system responses
- Hormonal fluctuations after birth
- Retained placental tissue
- A history of gestational hypertension or chronic high blood pressure
- Conditions like gestational diabetes
Women who had gestational hypertension during pregnancy are at greater risk of developing severe hypertension after childbirth. This can place significant strain on the heart, liver, and kidneys, and in rare cases, may lead to stroke, seizure, or organ failure if not treated promptly.
Recognizing the warning signs of postpartum preeclampsia is crucial. Symptoms such as severe headaches, visual disturbances, swelling, rapid weight gain, elevated blood pressure, and difficulty breathing should never be brushed off as “normal” postpartum discomfort. These signs warrant immediate medical care to prevent serious complications and ensure maternal safety.
Symptoms of Postpartum Preeclampsia
Knowing the signs of postpartum preeclampsia could save your life:
- Severe headache (often described as a preeclampsia headache postpartum)
- Swelling in hands, feet, or legs due to excess fluid
- High blood pressure (above the preeclampsia blood pressure range postpartum, typically 140/90 or higher)
- Vision changes (blurred vision or light sensitivity)
- Shortness of breath caused by pulmonary edema
- Upper abdominal pain
- Nausea or vomiting
- Sudden weight gain
Many of these can be mistaken for “normal” postpartum changes. But postpartum preeclampsia symptoms are serious. If something feels off—listen to your body and reach out to your healthcare provider immediately.
Ignoring the signs or symptoms, can lead to serious complications including damage to vital organs, heart disease, and more.
How Common Is Postpartum Preeclampsia?
It’s estimated that postpartum preeclampsia affects about 0.3% to 0.5% of all births. While that may seem rare, it’s severe postpartum preeclampsia cases like Chelsea’s that make early recognition and treatment vital.
Even high-profile women like Meghan Markle have brought attention to preeclampsia and related maternal health complications. Despite medical advances, the U.S. still ranks poorly for maternal health outcomes, and postpartum preeclampsia death is a stark reality for some.
How Serious Is Postpartum Preeclampsia?
Very. If left untreated, it can lead to stroke, seizures, heart failure, kidney damage, or death. That’s why early intervention is key. The postpartum preeclampsia survival rate is high when caught and treated—but timing is everything.
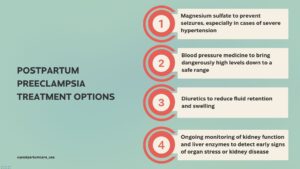
How to Treat Postpartum Preeclampsia
Postpartum preeclampsia treatment typically begins with prompt medical intervention, which is essential to prevent life-threatening complications like seizures, stroke, or organ failure. The main goals of treatment are to reduce blood pressure, prevent seizures, and protect vital organs—particularly the liver and kidneys.
Treatment options may include:
- Magnesium sulfate (often administered as a magnesium drip postpartum preeclampsia) to prevent seizures, especially in cases of severe hypertension
- Blood pressure medicine to bring dangerously high levels down to a safe range
- Diuretics to reduce fluid retention and swelling
- Ongoing monitoring of kidney function and liver enzymes to detect early signs of organ stress or kidney disease
In more severe cases or when symptoms don’t respond to outpatient care, hospitalization may be required to ensure close observation and aggressive treatment.
How Long Does Postpartum Preeclampsia Last?
The duration of postpartum preeclampsia can vary. For many women, blood pressure stabilizes and symptoms resolve within a few days to a few weeks. However, in others—especially those with complications or pre-existing conditions—how long preeclampsia symptoms last after pregnancy can depend on individual recovery and response to treatment. In rare cases, ongoing hypertension or kidney disease may require long-term management.
Postpartum Preeclampsia Recovery
The recovery process extends beyond physical healing. Many women report lingering feelings of fear, guilt, or trauma—especially if their diagnosis came unexpectedly or required an ICU stay.
Some important steps for postpartum preeclampsia recovery include:
- Regular follow-ups with your OB-GYN or primary care provider
- Continued blood pressure monitoring at home or in the clinic
- Adopting a postpartum preeclampsia diet rich in whole foods, fiber, and low in sodium to support cardiovascular and kidney health
- Addressing emotional well-being through therapy, support groups, or counseling if needed
Women may also need to continue blood pressure medication or other therapies long-term, depending on their recovery and any lingering symptoms of postpartum hypertension.
Does Postpartum Preeclampsia Go Away?
Yes—for most women, postpartum preeclampsia improves with prompt treatment and proper follow-up care. However, this condition should never be taken lightly.
Women who experience preeclampsia in the postpartum period have an elevated risk of:
- High blood pressure later in life
- Cardiovascular disease
- Preeclampsia after delivery in future pregnancies
This is why follow-up care in the postpartum period matters. Even after the immediate danger passes, staying proactive with your health can reduce the risk of future complications.
How to Protect Yourself
1. Learn the Symptoms
Bookmark this post. Share it with your partner or a loved one. Print it if you need to.
If you delivered in a hospital, your discharge nurse should review all of these symptoms of postpartum preeclampsia with you, but we are often exhausted and in such a rush to get home that it may go in one ear and out the other!
2. Monitor Your Health
Check your blood pressure regularly, especially in the first 6 weeks postpartum.
3. Ask for Help
Don’t downplay your symptoms. Don’t let fear of being “dramatic” stop you from speaking up. Your baby needs a healthy you. Prompt treatment is essential for your survival!
Don’t Ignore the Warning Signs
How do you treat postpartum preeclampsia? By treating your symptoms seriously. By listening to your intuition. By knowing that scary symptoms don’t mean you’re weak or failing—they mean your body is signaling for help.
If you’ve experienced postpartum preeclampsia, or are recovering from pre-eclampsia after delivery, know this: you are not alone. And if you’re reading this to prepare for your postpartum journey—good for you.
When it comes to preeclampsia vs postpartum hypertension, symptoms can overlap, but both require medical attention. Don’t wait.
Pin This for Later:
Postnatal Depletion
Meet the Team
Our Services
Supplements
A virtual healthcare clinic that helps postpartum mamas recover from postnatal depletion syndrome with a holistic approach.

Get in touch