Postpartum pelvic floor therapy is essential for new mothers recovering from childbirth. This therapy helps strengthen the pelvic floor muscles and alleviate symptoms such as urinary leakage, pain, and discomfort. In this guide, we’ll explore the benefits, techniques, and timelines of postpartum pelvic floor therapy to help you regain strength and improve your quality of life.
Key Takeaways
- Postpartum pelvic floor disorders, including incontinence and pelvic organ prolapse, can negatively impact a woman’s health and quality of life, making awareness and seeking treatment crucial.
- Pelvic floor physical therapy provides tailored support that not only addresses physical symptoms but also offers emotional guidance, enhancing recovery for new mothers.
- Early identification and intervention of pelvic floor issues are essential for effective treatment, with therapy typically recommended to begin four weeks post-delivery for optimal results.
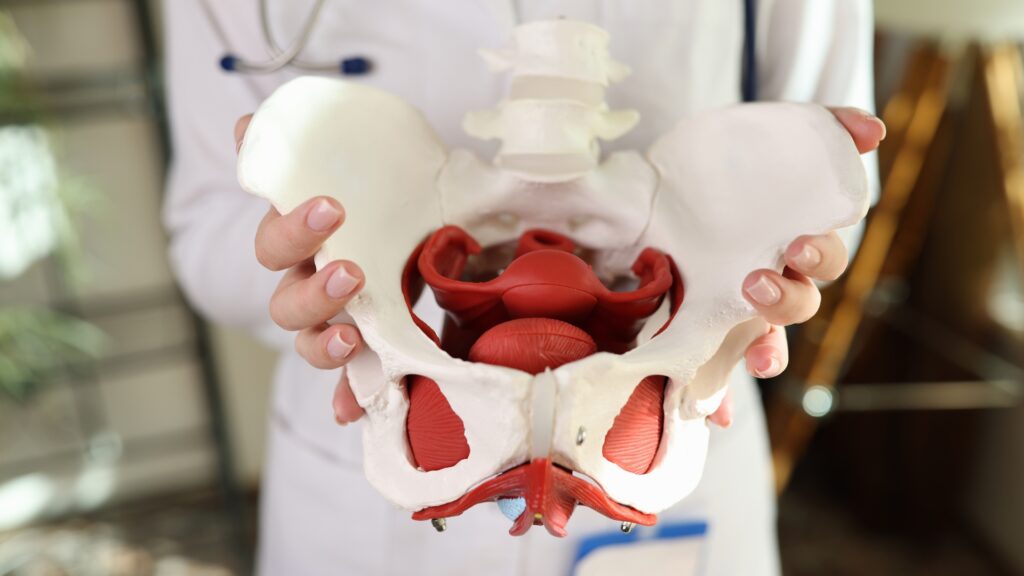
Understanding Postpartum Pelvic Floor Disorders
Postpartum pelvic floor disorders are conditions that affect the muscles and connective tissues in the pelvic region after childbirth (Source). These disorders can manifest in various ways, making it crucial for new mothers to understand the postpartum pfd symptoms and seek appropriate treatment. Common symptoms include:
- Urinary leakage and urgency
- Perineal pressure
- Pelvic organ prolapse
- Chronic pelvic pain
The types of disorders that can occur postpartum include urinary or fecal incontinence, pelvic organ prolapse, and diastasis recti. These conditions can significantly impact a woman’s health and quality of life post-childbirth. For instance, pelvic organ prolapse involves the descent of pelvic organs, such as the bladder, uterus, or rectum, into or outside of the vaginal canal, causing discomfort and functional issues.
Understanding how these pelvic floor disorder affect the pelvic floor muscles is essential. The pelvic floor is a group of muscles and connective tissues that support the pelvic organs and maintain continence. Childbirth, especially vaginal delivery, can stretch and weaken these muscles, leading to pelvic floor dysfunction. This dysfunction can manifest in various symptoms that disrupt daily life and overall well-being.
Recognizing the signs of postpartum pelvic floor disorders is the first step towards recovery. Ignoring these symptoms can lead to worsening conditions, making it vital for new mothers to seek professional evaluation and treatment. Understanding these disorders empowers women to take proactive steps towards restoring pelvic health and enhancing their quality of life.
Importance of Pelvic Floor Physical Therapy Post-Childbirth
Pelvic floor physical therapy plays a pivotal role in the recovery process post-childbirth. The primary goal of this therapy is to reduce the symptoms of pelvic floor disorders, increase muscle strength and endurance, and improve the overall quality of life for new mothers. Given the significant impact these disorders can have, professional evaluation by a physical therapist is essential.
Many women are unaware of their pelvic floor muscle function and may not realize the extent of their dysfunction. A physical therapist conducts a thorough assessment to tailor therapy to address specific pelvic floor issues. This personalized approach ensures that the treatment is effective and targets the unique needs of each patient.
Beyond physical recovery, pelvic floor therapy provides emotional support, helping mothers cope with the challenges of postpartum recovery. The therapy sessions offer a safe space for women to discuss their concerns and receive compassionate care. Early intervention is crucial, as it can mitigate the risks of long-term pelvic floor issues and enhance the overall recovery experience.
How to Identify Postpartum Pelvic Floor Issues
Identifying postpartum pelvic floor issues early on is crucial for timely intervention and effective treatment. Many women report feelings of vaginal pressure or fullness as early signs of pelvic floor dysfunction, which can be completely normal. This sensation may be accompanied by other symptoms, indicating the need for professional evaluation.
Leaking urine during activities like coughing, sneezing, or exercising is a fairly common symptom indicative of stress urinary incontinence. Additionally, difficulties in controlling gas, urine, or stool can signal pelvic floor disorders, including urinary and fecal incontinence. These symptoms can significantly affect a woman’s quality of life, making it essential to recognize and address them promptly.
Discomfort during intercourse is another potential sign of pelvic floor dysfunction. Women experiencing frequent urination, sometimes with urgency, should also consider it a potential indicator of pelvic floor issues and pelvic health concerns. Ignoring these symptoms can lead to worsening conditions, underscoring the importance of seeking professional evaluation and treatment early on.
Benefits of Pelvic Floor Therapy for New Mothers
Postpartum pelvic floor therapy offers numerous benefits for new mothers, especially after giving birth. It addresses dysfunctions ranging from mild discomfort to significant issues like incontinence and prolapse, enhancing overall well-being.
The therapy often includes a combination of exercises, electrical stimulation, biofeedback training, manual therapy, and education on behavioral modifications.
Personalized Treatment Plans
Pelvic floor specialists create individualized treatment strategies based on comprehensive evaluations of each mother’s specific needs. This personalized approach ensures that the therapy addresses the unique challenges and goals of each patient, enhancing its effectiveness.
The first session typically ends with your physical therapist providing a detailed treatment plan based on the assessment. A home exercise program may also be introduced during the first appointment to aid in recovery, allowing mothers to continue their progress between sessions.
Strengthening Pelvic Floor Muscles
Strengthening the pelvic floor muscles is a core component of pelvic floor therapy. Kegel exercises involve:
- Systematically tightening and relaxing the pelvic floor muscles
- Being commonly taught to improve strength and control
- Being adaptable for different levels of pelvic floor dysfunction, ensuring that each patient gets the most benefit.
Biofeedback can enhance awareness of pelvic floor muscle function by:
- Helping patients learn to contract and relax these muscles more effectively.
- Aiding in reducing muscle tension and improving coordination by monitoring muscle activity in real time.
- Providing tangible feedback through devices, allowing individuals to visualize their pelvic floor muscle activity and improve control.
Electrical stimulation therapy can be particularly beneficial for patients with weakened pelvic floor muscles or those experiencing pain. The application of electrical stimulation may enhance muscle recovery and increase the effectiveness of pelvic floor exercises. Reverse Kegel exercises, which help in relaxing pelvic floor muscles, provide a counterbalance to tightening exercises and are an integral part of a comprehensive therapy plan.
Improving Quality of Life
Pelvic floor therapy can significantly improve a new mother’s quality of life by alleviating pelvic pain, including discomfort during daily activities and sexual intimacy. Incorporating electrical stimulation can enhance recovery by promoting muscle contractions and potentially alleviating discomfort.
Overall, pelvic floor therapy not only addresses specific issues like pain and incontinence but enhances general well-being, allowing new mothers to engage more fully in life. Therapy helps mothers regain confidence and enjoy their postpartum period more fully, as it can reduce pain and improve physical activity levels.
Common Techniques Used in Pelvic Floor Physical Therapy
Postpartum pelvic floor therapy typically includes a variety of techniques. These methods, which range from exercises to advanced technological interventions, are designed to address different aspects of pelvic floor dysfunction and enhance the effectiveness of the therapy.
Pelvic Floor Exercises
Kegel exercises involve systematically tightening and relaxing the pelvic floor muscles to improve strength and control. These exercises are widely recognized for their effectiveness in strengthening the pelvic floor muscles, requiring patients to contract and relax these muscles regularly.
Regular pelvic floor exercises can significantly enhance pelvic floor muscle strength and prevent future issues related to pelvic dysfunction. Incorporating pelvic floor training into routine exercise is essential for sustaining pelvic health over the long term.
Biofeedback Training
Biofeedback devices allow patients to monitor and evaluate their progress, providing tangible feedback on muscle control. This therapy is utilized in pelvic floor muscle training to enhance control over these muscles, making exercises more effective.
Improving muscle control through biofeedback training can lead to better management of pelvic floor disorders, enhancing quality of life. By offering real-time feedback, these devices help patients learn to contract and relax their pelvic floor muscles more effectively, ensuring optimal results from their exercises.
Electrical Stimulation
Electrical stimulation is a technique used in pelvic floor therapy to enhance muscle contractions, providing a way to strengthen pelvic floor muscles. This method supports recovery from various pelvic floor disorders by promoting muscle activity and aiding in muscle strengthening.
Enhancing muscle contractions, electrical stimulation can improve muscle control and support the overall recovery process. This technique is particularly beneficial for patients with weakened pelvic floor muscles or those experiencing pain, making it a valuable component of comprehensive pelvic floor therapy.
Timing and Duration of Postpartum Pelvic Floor Therapy
Pelvic floor physical therapy is typically suggested to start around four weeks after delivery, but can begin as early as 1 to 3 days after delivery. Early intervention is crucial for mitigating the risks of long-term pelvic floor issues and enhancing overall recovery.
Therapy typically consists of eight to twelve sessions, conducted over a span of three to four months to aim at restoring pre-pregnancy activity levels, often within six weeks. This structured approach ensures that many mothers receive adequate support throughout their recovery journey.
Patients generally see an improvement in muscle strength by one grade within two to three weeks of starting therapy. Consistent therapy sessions and adherence to the treatment plan are key to achieving optimal results and restoring pelvic floor health.
Preparing for Your First Pelvic Floor Therapy Session
Preparing for your first pelvic floor therapy session involves a few practical steps. Completing a health questionnaire and consent form online before your session helps maximize treatment time. This preparation ensures that the therapist has all the necessary information to tailor the therapy to your specific needs.
It’s advisable to wear loose and comfortable clothing to your first therapy session. Arriving at least 15 minutes early can ensure a smooth intake process and start to your session.
Remember, you can opt out of any part of the pelvis examination at any time, including the internal assessment.
The Role of Urogynecology in Postpartum Recovery
Urogynecologists play a crucial role in postpartum recovery by:
- Working alongside physical therapists to create a multidisciplinary approach for managing pelvic floor disorders.
- Collaborating to improve patient outcomes in pelvic floor rehabilitation.
- Integrating urogynecological assessments to ensure physical therapy addresses specific pelvic floor dysfunctions effectively.
- Helping manage symptoms of pelvic floor disorders, allowing women to return to their daily routines.
Postpartum pelvic floor dysfunction can significantly affect a woman’s emotional and sexual health. Many women experience psychological stress due to pelvic floor dysfunction symptoms during and after pregnancy, making the role of urogynecologists vital in addressing both physical and emotional aspects of recovery.
Emotional and Psychological Support During Therapy
Pelvic floor physical therapy is grounded in a whole-person, individualized care philosophy in a supportive environment. New mothers can expect to gain a better understanding of healing and preventing pelvic floor dysfunctions through pelvic floor pt therapy.
Pelvic floor physical therapists educate mothers about the anatomy, function, and health maintenance of the pelvic floor, increasing their awareness and empowerment. This compassionate support and guidance are essential for a positive therapy experience and successful recovery.
Long-Term Pelvic Health Maintenance
Follow-up appointments with a physical therapist can help monitor progress and adjust treatment plans as needed for ongoing pelvic health services and pelvic physical therapy. These check-ins ensure that any emerging issues are addressed promptly and effectively by a doctor.
Urogynecologists may recommend pelvic floor muscle training as a preventative measure for pelvic organ prolapse. Postpartum women may benefit from repeated pelvic floor therapy after multiple births due to increasing symptoms. Maintaining a proactive approach to pelvic health ensures long-term well-being and function for new mothers.
Summary
Pelvic floor therapy is a vital part of postpartum recovery, offering numerous benefits such as improved muscle strength, reduced pain, and enhanced quality of life. By understanding the importance of pelvic floor health and recognizing the symptoms of dysfunction, new mothers can take proactive steps to ensure their well-being.
Seeking professional evaluation and embracing a personalized treatment plan can make a significant difference. With the support of physical therapists and urogynecologists, new mothers can navigate their postpartum journey with confidence and reclaim their health and vitality.
Frequently Asked Questions
When should I start pelvic floor physical therapy after childbirth?
It is generally recommended to start pelvic floor physical therapy around four weeks after childbirth, although you may begin as early as 1 to 3 days postpartum if needed. Prioritizing this therapy can significantly aid in recovery.
What are the common symptoms of postpartum pelvic floor disorders?
Common symptoms of postpartum pelvic floor disorders include urinary leakage and urgency, perineal pressure, pelvic organ prolapse, chronic pelvic pain, and difficulty controlling gas, urine, or stool. Discomfort during intercourse is also a notable symptom.
How long does pelvic floor physical therapy usually last?
Pelvic floor physical therapy usually lasts between three to four months, comprising eight to twelve sessions aimed at restoring function.
What techniques are commonly used in pelvic floor physical therapy?
Pelvic floor physical therapy commonly employs techniques such as Kegel exercises, biofeedback training, electrical stimulation, manual therapy, and behavioral education. These methods effectively aid in strengthening pelvic muscles and improving overall function.
How can I prepare for my first pelvic floor therapy session?
To effectively prepare for your first pelvic floor therapy session, complete any required health questionnaires and consent forms online beforehand, wear loose and comfortable clothing, and aim to arrive at least 15 minutes early. Additionally, remember that you can opt out of any part of the examination if you choose.
If you need a referral, we have a great network of physical therapists that offer treatment both virtually and in-person throughout the US. Reach out for more info!
Pin This for Later:

Postnatal Depletion
Meet the Team
Our Services
Supplements
A virtual healthcare clinic that helps postpartum mamas recover from postnatal depletion syndrome with a holistic approach.


Get in touch