If you’re navigating postpartum life and something still feels “off,” it’s not all in your head. Fatigue, hair loss, mood swings, or persistent anxiety may be more than just typical new mom stress. For some women, these symptoms could be early signs of Hashimoto’s thyroiditis, a chronic autoimmune thyroid disorder that’s more common than many realize.
Let’s walk through what Hashimoto’s is, how it shows up in postpartum women, and what to do if you suspect something more is going on than just “new mom exhaustion.”
What Is Hashimoto’s Thyroiditis?
Hashimoto’s thyroiditis is an autoimmune condition in which the immune system mistakenly attacks the thyroid gland, leading to chronic inflammation and eventually hypothyroidism. It’s one of the most common causes of an underactive thyroid, especially in women. In fact, women are up to 10 times more likely than men to be diagnosed with it, and postpartum women are particularly vulnerable (Source).
During pregnancy, your immune system shifts to protect your growing baby. After birth, as your body recalibrates, your immune system can rebound aggressively—and for some women, this triggers autoimmune conditions like Hashimoto’s.
Symptoms of Hashimoto’s in Postpartum Women
Hashimoto’s can present subtly at first, which is why it often gets brushed off as “just postpartum.” But symptoms of hypothyroidism and Hashimoto’s can significantly affect your physical and mental health. Common symptoms include:
- Fatigue that doesn’t improve with rest
- Hair loss or thinning
- Weight gain or difficulty losing weight
- Cold intolerance
- Constipation
- Brain fog or difficulty concentrating
- Low libido
- Mood changes like postpartum depression or anxiety
- Irregular or heavy periods
- Hoarseness or pressure in the neck
If you’re dealing with several of these symptoms, it’s worth digging deeper—especially if you had postpartum depression or anxiety that isn’t resolving, or if you’re experiencing things like cold intolerance, dry skin, and sluggishness despite “doing everything right.”
How Hashimoto’s Is Diagnosed
If you had your thyroid levels tested during pregnancy, you’re not alone. It’s fairly standard prenatal care.
But what’s not standard? Testing your thyroid levels postpartum—despite the fact that many women experience significant blood loss during birth, which can affect thyroid hormone conversion and overall function.
A full thyroid panel should include:
- TSH (Thyroid Stimulating Hormone)
- Free T4 and Free T3 (thyroid hormones)
- Anti-TPO and Anti-TG antibodies (to detect autoimmune thyroid disease)
Note: It’s possible to have Hashimoto’s with normal thyroid hormone levels, especially early in the disease, so antibody testing is important.
The Connection Between Hashimoto’s, Mental Health, and Fertility
One of the most overlooked connections is between low thyroid function and postpartum mental health.
Low thyroid function can mimic or contribute to postpartum depression and postpartum anxiety. You might feel irritable, exhausted, overwhelmed, and emotionally detached—symptoms often blamed on new motherhood, but in reality, linked to low thyroid hormone levels.
There’s also a link between Hashimoto’s and fertility. Hashimoto’s can disrupt ovulation and menstrual regularity, making it harder to conceive in the future.
Postpartum Thyroiditis vs. Hashimoto’s
It’s also important to distinguish Hashimoto’s from another condition called postpartum thyroiditis. Postpartum thyroiditis causes a temporary inflammation of the thyroid after giving birth, and it can look similar to Hashimoto’s early on.
The difference? Postpartum thyroiditis is usually temporary and doesn’t always require long-term medication. Hashimoto’s is chronic and typically requires ongoing management with thyroid hormone replacement according to most physicians in the US.
However, by doing the Postpartum Care USA protocol, I was able to cure myself of Hashimoto’s (and help many other moms in the same situation!) Click here to hear more about my story.
The Role of Nutrient Deficiency in Hashimoto’s
Nutrient deficiencies can make Hashimoto’s symptoms worse. After giving birth, many women experience postpartum iron deficiency anemia or low levels of nutrients like selenium, zinc, and vitamin D.
Low iron, in particular, is a big deal. Iron is essential for thyroid hormone production and conversion. Low iron after birth—especially for those who had postpartum hemorrhage or low iron during pregnancy—can cause symptoms like:
- Fatigue
- Insomnia
- Hair loss
- Low mood or increased postpartum anxiety and depression
Restoring iron levels can be a game changer for your energy, mental clarity, and mood. (Learn more in our blog post on postpartum iron deficiency.)
Treatment of Hashimoto’s in Postpartum Women
Standard treatment usually involves thyroid hormone replacement. The most common is Synthroid (levothyroxine), which provides T4—the storage form of thyroid hormone. Some women feel better adding T3 (the active form) or using natural desiccated thyroid (like Armour) that contains both T4 and T3.
There’s no one-size-fits-all approach. Some women with Hashimoto’s still feel tired and foggy on T4 alone. Working with a provider who understands functional ranges and personalizes treatment is key.
What Most Providers Won’t Tell You About Getting Off of Synthroid (Levothyroxine)
If you’ve ever been told you’ll need Synthroid—or any form of levothyroxine—for the rest of your life, you’re not alone. That’s the message most women hear once they’re diagnosed with Hashimoto’s or hypothyroidism. But here’s what most providers won’t tell you: healing your thyroid naturally is possible. I know, because I did it myself.
Within just six months of working on the root causes of my symptoms—nutrient depletion, chronic stress, gut inflammation—I was able to reverse my Hashimoto’s, lower my antibodies, and get off Synthroid for good.
The truth is, thyroid medication is often handed out like a long-term solution, but rarely does it come with an explanation of why your thyroid is struggling in the first place. At Postpartum Care USA, we believe your thyroid deserves more than a bandaid fix. It deserves a full-body approach that focuses on nourishment, healing, and long-term wellness.
The Food-First Approach
Your thyroid needs certain nutrients to function properly—especially after the stress of pregnancy, delivery, or chronic postpartum depletion. We focus heavily on supporting your thyroid with real food, not just pills.
Here are some of the thyroid-supporting nutrients we prioritize:
- Iron (for oxygen transport and hormone synthesis): leafy greens, red meat, legumes, fruit, tofu
- Magnesium (for stress response and energy): dark chocolate, avocado, seeds, leafy greens
- Zinc (for hormone production and immune support): shellfish, legumes, poultry
- Iodine (for thyroid hormone creation): eggs, seafood, whole grains
- Selenium (for thyroid hormone conversion and antioxidant support): Brazil nuts, oatmeal, seeds
- B Vitamins (for energy and hormone regulation): liver, salmon, leafy greens, eggs, milk
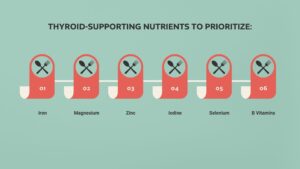
When we rebuild from the inside out, we can often restore thyroid function without life-long medication.
But It’s Not Just About Food…
Autoimmune thyroid conditions like Hashimoto’s often stem from gut health issues and systemic inflammation. If the gut lining is inflamed—whether from stress, lack of sleep, food sensitivities, or blood sugar imbalance—your immune system can go into overdrive, triggering thyroid antibodies.
We test for these antibodies (anti-TPO and anti-TG), because you can still have Hashimoto’s even if your TSH is “normal.” And when antibodies are high, we take a full-body approach that includes:
- Limiting inflammatory foods (gluten and dairy are common triggers)
- Improving cortisol metabolism (aka managing stress and restoring nervous system balance)
- Balancing blood sugar (no more skipping meals or chasing intermittent fasting trends)
- Healing the gut lining
- Testing for full thyroid panels—not just TSH, but also Free T3, Free T4, reverse T3, and both antibodies
A Word on Thyroid Medications
We’re not anti-medication—but we are anti-one-size-fits-all. Most women are prescribed standard levothyroxine (like Synthroid), which often contains fillers like gluten or lactose, and doesn’t actually improve symptoms for many.
Once you start on Synthroid, your body can become dependent on it—especially if you haven’t addressed the underlying root causes. That’s why at PPCU, when medication is truly needed, we prefer compound thyroid medications that can be tailored to your body and support both symptoms and thyroid function.
But here’s the exciting part: with the right care, many of our patients are able to wean off of medication entirely and regain energy, clarity, fertility, and emotional balance—all without synthetic hormone dependency.
You Deserve More Than “Just Take This Pill”
If you’re feeling dismissed, unheard, or still unwell despite being told your thyroid labs are “normal,” we’re here to say: you are not crazy—and you are not stuck.
At Postpartum Care USA, we treat your thyroid holistically by:
- Addressing root-cause inflammation and adrenal health
- Testing properly and tracking your full thyroid picture
- Supporting your gut and nutrient absorption
- Guiding you toward nourishing, blood-sugar-balancing meals
- Rebuilding your energy reserves and nervous system
You deserve a provider who sees the whole you—not just a number on a lab report.
Mama, if you’re tired, anxious, foggy, cold, gaining weight, losing hair, or just feel like you’re not yourself…we will help you figure out why. And we’ll walk with you every step of the way.
Diet and lifestyle changes also play a big role. Many postpartum women benefit from:
- A gluten-free, anti-inflammatory diet
- Blood sugar balancing meals
- Managing stress and supporting adrenal health
- Gut healing protocols (since 70% of the immune system is in the gut)
Long-Term Complications of Hashimoto’s If Left Untreated
If left untreated, postpartum Hashimoto’s thyroiditis can lead to serious complications, including:
- Goiter (enlarged thyroid gland)
- Chronic postpartum fatigue
- Worsening postpartum depression or anxiety
- Fertility struggles in future pregnancies
- Increased risk of birth defects if untreated before a subsequent pregnancy
- Cardiovascular risks from prolonged hypothyroidism
- Myxedema (a rare but life-threatening complication of severe hypothyroidism)
Hashimoto’s and Autoimmune Overlap
Hashimoto’s often doesn’t show up alone. If you’ve been diagnosed with other autoimmune conditions—like rheumatoid arthritis, celiac disease, or lupus—you may be more likely to develop Hashimoto’s. There’s also a genetic component, so if thyroid issues run in your family, that’s another important clue.
When to Get Help for Hashimoto’s Thyroiditis Postpartum
If you’re experiencing symptoms that don’t improve with sleep, nutrition, or time—and especially if you’ve already had iron or thyroid issues during pregnancy—it’s time to get tested.
Hashimoto’s thyroiditis affects millions of women, many of whom are struggling silently during the postpartum period. You deserve more than “just wait it out” or “this is just what motherhood feels like.”
Get the labs. Ask the questions. Advocate for your energy and your well-being. Because when you feel better, everything changes—not just for you, but for your family, too.
If this resonated with you or you’re curious about testing, treatment options, or natural strategies to manage postpartum thyroid symptoms, reach out or check out our resource library. You don’t have to go through this alone.
Pin This for Later:


Postnatal Depletion
Meet the Team
Our Services
Supplements
A virtual healthcare clinic that helps postpartum mamas recover from postnatal depletion syndrome with a holistic approach.

Get in touch